Drug-Induced Lupus Risk Calculator
Medication Risk Assessment
Risk Assessment Results
Your risk will be displayed here after calculation
Expected Symptom Timeline
Symptoms typically appear:
Most common timeframe for symptom onset
Range varies based on individual factors
Recovery Timeline After Stopping Medication
80% of people see significant improvement
95% of people recover fully
Most people don’t realize that a common blood pressure pill, an antibiotic, or even a treatment for arthritis could trigger a lupus-like illness. This isn’t the same as systemic lupus erythematosus - the chronic autoimmune disease most people know about. This is drug-induced lupus, a reversible condition caused by certain medications. It mimics lupus symptoms but usually disappears once you stop the drug. The problem? Many doctors miss it. Patients suffer for months, misdiagnosed with fibromyalgia, chronic fatigue, or even aging. If you’re over 50, taking long-term medication, and suddenly feel tired, achy, and feverish, this could be why.
What Does Drug-Induced Lupus Actually Feel Like?
You won’t get the classic butterfly rash across your cheeks like in classic lupus. That happens in less than 15% of drug-induced cases. Instead, the symptoms are quieter, more general - and easily mistaken for something else.
- Joint pain and swelling - affects 65-75% of people. Often in the hands, knees, or wrists. Feels like arthritis, but without long-term damage.
- Muscle aches - reported in 75-85% of cases. Not just soreness - deep, persistent pain that doesn’t improve with rest.
- Fever without infection - low-grade, recurring. Often above 100.4°F (38°C), with no clear source.
- Extreme fatigue - 80-90% of patients say they’re worn out, even after sleeping.
- Chest pain when breathing - this is serositis. Inflammation around the lungs (pleuritis) or heart (pericarditis). It’s sharp, gets worse when you inhale deeply.
- Weight loss - 30-40% lose weight without trying. Not from dieting. Just from feeling unwell.
Here’s what’s different from regular lupus: kidneys and brain are rarely involved. Less than 5% of drug-induced cases affect the kidneys. In regular lupus, it’s 30-50%. Nervous system problems like seizures or confusion? Under 3% in drug-induced lupus. That’s a big clue.
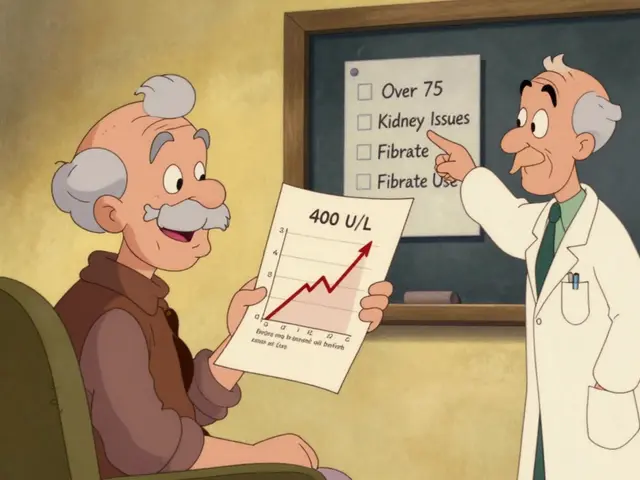
Which Medications Cause It?
It’s not random. Certain drugs have a known link. The risk isn’t high for most people - but it’s real, and it builds up over time.
- Hydralazine (for high blood pressure): 5-10% of long-term users develop it. Risk jumps to 20% if you’re a slow acetylator (a genetic trait).
- Procainamide (for irregular heartbeat): Up to 30% of people on it for over a year get drug-induced lupus. That’s why it’s rarely used today.
- Minocycline (an acne antibiotic): Causes lupus-like symptoms in 1-3% of users. Often reversible when switched to doxycycline.
- TNF-alpha inhibitors (like etanercept or infliximab): Used for rheumatoid arthritis, Crohn’s, psoriasis. These have become the fastest-growing cause since 2015. About 12-15% of new DIL cases now come from these drugs.
- Immune checkpoint inhibitors (like pembrolizumab): Used in cancer treatment. Around 1.5-2% of patients develop lupus-like symptoms.
It usually takes 3 to 6 months of continuous use before symptoms show up. Sometimes it’s as short as 3 weeks, or as long as 2 years. The longer you’re on the drug, the higher the risk. That’s why it’s often missed - doctors don’t connect a symptom that shows up after a year of treatment to a pill you’ve been taking since day one.
How Is It Diagnosed?
There’s no single test. Diagnosis is a puzzle made of three pieces: your meds, your symptoms, and your blood.
First, your doctor needs your full medication history - every pill, even over-the-counter ones. Many patients don’t realize supplements or antibiotics could be the trigger. Be ready to list everything you’ve taken in the last 2 years.
Then, blood tests:
- ANA (antinuclear antibody): Positive in over 95% of drug-induced lupus cases. But this test is also positive in healthy people and other autoimmune diseases. So it’s not enough on its own.
- Anti-histone antibodies: This is the key. Found in 75-90% of drug-induced cases. In regular lupus, only 50-70% have them. If you’re ANA-positive AND anti-histone positive - that’s a strong signal.
- Anti-dsDNA antibodies: These are usually negative in drug-induced lupus. In regular lupus, they’re positive in 60-70% of cases. If yours are negative, it’s another clue.
- ESR and CRP: These measure inflammation. They’re often elevated, confirming your body is in a flare-up state.
Doctors also rule out other causes: infections, other autoimmune diseases, even cancer. If your symptoms improve after stopping the drug, that’s the final piece of proof.
What Happens When You Stop the Drug?
This is the good news: drug-induced lupus usually goes away.
After stopping the trigger medication:
- 80% of people feel significantly better within 4 weeks.
- 95% recover fully within 12 weeks.
- Most symptoms - joint pain, fever, fatigue - fade fast.
But recovery isn’t always instant. Some people need help along the way.
- NSAIDs (like ibuprofen): Used for mild joint pain and inflammation. Works for 60-70% of cases.
- Low-dose steroids (prednisone): If symptoms persist, a short course (5-10 mg daily for 4-8 weeks) clears them up in 85-90% of cases.
- Immunosuppressants (like azathioprine): Only needed in rare cases where symptoms linger beyond 3 months. Most people never need these.
One patient on Reddit stopped hydralazine after 18 months and saw 80% improvement in 4 weeks. Another switched from minocycline to doxycycline for acne - joint swelling vanished in 3 weeks. These aren’t rare stories. They’re the norm.
Why Do Some People Get It and Others Don’t?
It’s not just the drug. Genetics play a big role.
If you’re a “slow acetylator,” your body processes certain drugs like hydralazine and procainamide slower than average. That means the drug lingers longer in your system, increasing the chance your immune system reacts to it. People with this trait have nearly a 5-fold higher risk of developing drug-induced lupus from hydralazine.
Another genetic factor: HLA-DR4. If you have this marker, your risk increases 3.2 times. These aren’t routine tests - but if you’ve had drug-induced lupus before, or if your family has autoimmune conditions, it’s worth asking about.
Age matters too. Most cases happen in people over 50. Younger people rarely get it. That’s why it’s often mistaken for normal aging or stress.
What About Long-Term Risks?
Once you stop the drug and symptoms fade, drug-induced lupus usually doesn’t come back. But there are two important warnings.
First: if you’ve had it once, you’re at higher risk if you’re exposed to the same drug again. Never take it again. Even a small dose can trigger it faster.
Second: some people develop a different autoimmune disease later. It’s rare, but possible. That’s why ongoing check-ups with a rheumatologist are wise - not because DIL will return, but because your immune system has shown it can go off track.
Most people never need long-term treatment. No lifelong steroids. No chemotherapy. Just stopping the drug - and waiting.
What Should You Do If You Suspect It?
If you’re on one of these high-risk medications and have new symptoms:
- Write down every medication you’ve taken in the last 2 years - including doses and start dates.
- Track your symptoms: when they started, what makes them better or worse.
- Ask your doctor: “Could this be drug-induced lupus?” Don’t wait for them to bring it up.
- Request ANA and anti-histone antibody tests.
- If the drug is high-risk (like hydralazine or procainamide), ask about alternatives.
Don’t stop your medication on your own. Some of these drugs treat life-threatening conditions. Work with your doctor to switch safely.
For example: if you’re on hydralazine for high blood pressure, your doctor might switch you to lisinopril or amlodipine - both have no known link to lupus. If you’re on minocycline for acne, doxycycline is a safer alternative.
What’s Changing in Medicine?
Doctors are getting better at spotting this. The American College of Rheumatology updated its diagnostic guidelines in 2023 to make it clearer how to confirm drug-induced lupus.
Some European guidelines now recommend genetic testing (NAT2) before starting hydralazine in older patients. It’s not common in the U.S. yet - but it might be soon.
Researchers are also looking at blood markers - like specific microRNAs - that could predict who’s at risk before symptoms even appear. That could change how we prescribe these drugs in the future.
For now, the best defense is awareness. If you’re over 50, taking long-term meds, and feeling off - don’t assume it’s just getting older. Ask the question. Get the blood test. Your body might be trying to tell you something.
Can drug-induced lupus turn into regular lupus?
No, drug-induced lupus does not turn into systemic lupus erythematosus (SLE). They are two separate conditions. DIL is triggered by medication and resolves after stopping the drug. SLE is a chronic autoimmune disease with different causes and long-term progression. However, having DIL once may slightly increase your risk of developing another autoimmune condition later - but not specifically SLE.
How long does it take to recover from drug-induced lupus?
Most people start feeling better within 2 to 4 weeks after stopping the medication. About 80% see major improvement by 4 weeks, and 95% recover fully within 12 weeks. Symptoms like joint pain and fatigue fade first. In rare cases, symptoms last longer - but that’s usually because the drug wasn’t stopped early enough or another condition is present.
Is drug-induced lupus dangerous?
It’s serious but rarely life-threatening. Unlike regular lupus, it rarely affects kidneys, brain, or other major organs. The biggest danger is misdiagnosis. If it’s mistaken for SLE, patients might be put on strong immunosuppressants unnecessarily - which carry real risks like infections and cancer. Once the drug is stopped, the risk drops dramatically.
Can I take the same drug again if I had drug-induced lupus once?
Absolutely not. Re-exposure to the same drug almost always causes a faster, more severe recurrence. Even a small dose can trigger symptoms again within days. Once you’ve had drug-induced lupus from a specific medication, it’s permanently off-limits. Your doctor should note this in your medical record.
Are there any natural remedies that help?
There’s no proven natural cure. The only proven treatment is stopping the drug. Some people report feeling better with rest, low-sodium diets, or omega-3 supplements, but these don’t treat the underlying immune reaction. Avoid unproven supplements that claim to “boost immunity” - they could make things worse. Stick to medical advice and avoid self-treatment.
Who should I see if I suspect drug-induced lupus?
See a rheumatologist - a doctor who specializes in autoimmune diseases. Your primary care doctor can start the process with blood tests, but a rheumatologist knows how to interpret the results, rule out other conditions, and confirm the link to your medication. Don’t wait for a referral - ask for one if your symptoms persist.



Comments
Conor McNamara
November 17, 2025
so u know that hydralazine thing? i read somewhere the gov knows about this but keeps it quiet so pharma keeps makin cash... i been on it 14 months and my joints feel like rusted hinges... why no warning on the bottle? 🤔
steffi walsh
November 18, 2025
OMG this is so important!! I had this exact thing last year and thought I was just getting old 😭 switched from minocycline to doxycycline and my energy came back in 3 weeks. Don’t ignore those aches - your body’s screaming!
Leilani O'Neill
November 19, 2025
How is it possible that people in Ireland and the US are only now learning about this? We’ve known about procainamide-induced lupus since the 70s. It’s not a mystery - it’s negligence. If you’re over 50 and still on hydralazine, you’re either reckless or uneducated. And no, “natural remedies” won’t fix a pharmaceutical-induced autoimmune reaction.
Riohlo (Or Rio) Marie
November 20, 2025
Let’s be real - this isn’t ‘drug-induced lupus.’ It’s corporate malfeasance wrapped in a white coat. They knew. They knew the acetylator polymorphism was a thing. They knew the half-life risk profile. They kept pushing these drugs because the profit margin on biologics is 900%. And now we’re supposed to be grateful they didn’t kill us? The real tragedy isn’t the lupus - it’s that we still trust the system that made this happen.
And don’t get me started on ‘alternative remedies.’ If you think turmeric fixes immune dysregulation from TNF-alpha inhibitors, you’ve been scammed by a yoga instructor with a blog.
Kristi Joy
November 20, 2025
Thank you for sharing this - I’ve seen so many patients dismissed as ‘just tired’ or ‘anxious.’ This is a wake-up call for everyone on long-term meds. Please, if you’re reading this and feeling off, write down every pill you’ve taken. Bring it to your doctor. You deserve to be heard. You’re not imagining it.
Hal Nicholas
November 22, 2025
Wow. So now we’re blaming Big Pharma for people who can’t take care of themselves? If you’re over 50 and taking 12 pills a day, maybe stop popping everything and get off the couch. This isn’t a conspiracy - it’s poor lifestyle choices.
Louie Amour
November 22, 2025
LOL you think stopping a drug fixes it? You’re naive. The immune system doesn’t just reset like a phone. Once it’s triggered, you’re permanently damaged. And now you’re telling people to go off life-saving meds? What if their BP spikes? What if their heart goes haywire? You’re not helping - you’re endangering people with your half-baked Reddit wisdom.
And don’t get me started on ‘anti-histone antibodies.’ That’s not a diagnostic tool - it’s a statistical fluke. Real doctors use clinical judgment, not lab bingo.
Kristina Williams
November 22, 2025
They’re lying. This is all a ploy to sell more blood tests. I know a guy who stopped his meds and got worse. They just want you to pay for more tests. Don’t fall for it.
Write a comment