Pancreatic Stress Risk Calculator
Assess Your Stress Impact on Pancreatic Health
Based on scientific evidence linking chronic stress to pancreatic cancer biology, estimate your risk based on current habits. This tool calculates how well you're managing key stress pathways described in the article.
When you hear the word "stress," you probably picture a tight deadline or a traffic jam. Few people connect that everyday pressure to the silent killer lurking in the pancreas. Yet a growing body of science shows that chronic stress can tip the balance from a healthy pancreas to a malignant one, and it can speed up tumor growth once cancer is already present.
Key Takeaways
- Chronic psychological stress activates the hypothalamic‑pituitary‑adrenal (HPA) axis, flooding the body with cortisol and adrenaline.
- These stress hormones promote DNA damage, inflammation, and an immunosuppressive environment that favors pancreatic tumor initiation.
- Epidemiological studies consistently link high‑stress occupations and poor coping habits with a higher incidence of pancreatic cancer.
- Targeting stress pathways-through lifestyle changes, psychotherapy, or pharmacological agents-shows promise in slowing tumor progression.
- Patients can adopt a practical checklist to reduce stress‑related cancer risk without overhauling their entire lives.
Pancreatic Cancer is a malignant disease of the pancreas that accounts for about 3% of all cancers in the United States but causes roughly 10% of cancer deaths worldwide. Its stealthy onset, aggressive biology, and late diagnosis contribute to a five‑year survival rate under 10%. Stress refers to the physiological and psychological response to perceived threats or challenges triggers a cascade of hormonal and cellular events that can influence every step of pancreatic tumorigenesis.
How the Body Reacts to Chronic Stress
The brain‑body stress system centers on the HPA Axis a feedback loop involving the hypothalamus, pituitary gland, and adrenal cortex. When stressors persist, the hypothalamus releases corticotropin‑releasing hormone (CRH), prompting the pituitary to secrete adrenocorticotropic hormone (ACTH). ACTH then drives the adrenal cortex to pour out Cortisol the primary glucocorticoid hormone that regulates metabolism, immune function, and stress response. Simultaneously, the sympathetic nervous system spikes adrenaline (epinephrine) levels, preparing the “fight‑or‑flight” reaction.
In a healthy individual, these hormones rise and fall quickly, helping the body adapt. Chronic stress, however, flattens the rhythm, keeping cortisol and adrenaline elevated for hours or days. That prolonged exposure reshapes gene expression, damages DNA, and dampens immune surveillance-exactly the conditions cancer cells thrive in.
Molecular Links Between Stress Hormones and Pancreatic Cancer
Several pathways translate hormonal chaos into tumor‑friendly terrain:
- DNA Damage and Repair Suppression: Cortisol binds glucocorticoid receptors that can interfere with the p53‑mediated DNA repair machinery, increasing mutation rates in pancreatic ductal cells.
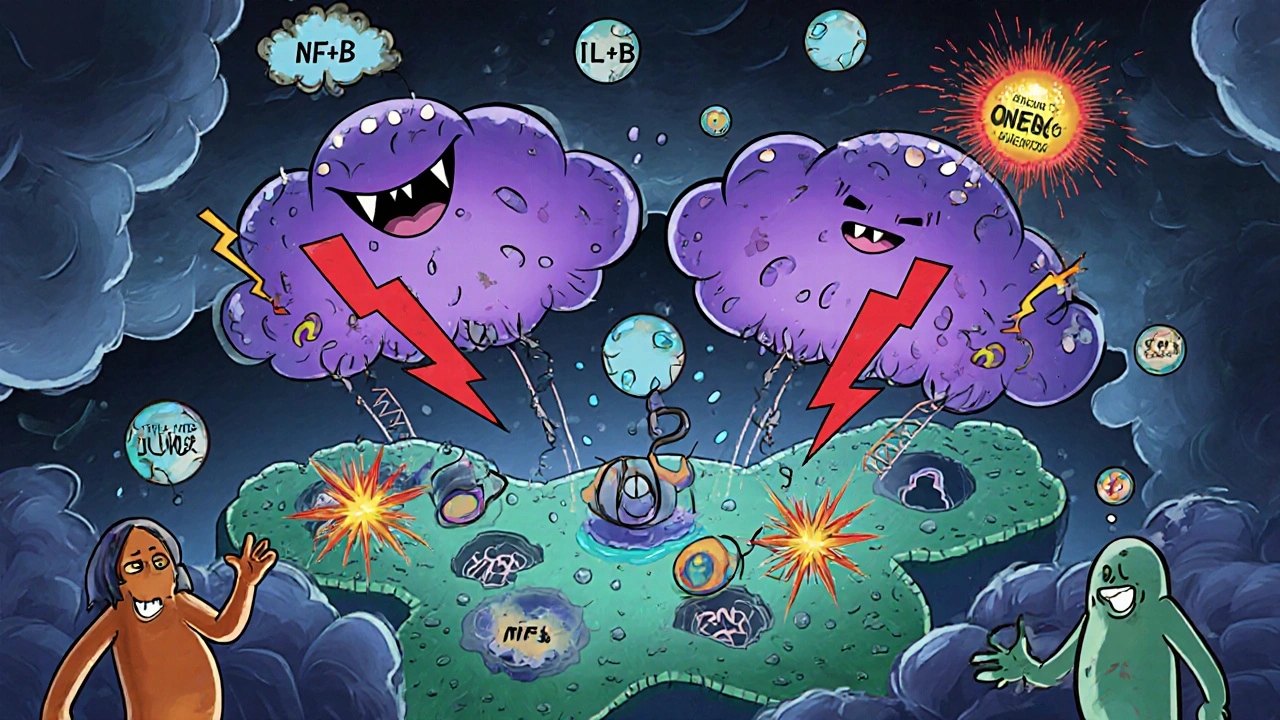
- Inflammation Amplification: Both cortisol (when dysregulated) and adrenaline stimulate NF‑κB, a transcription factor that drives production of pro‑inflammatory cytokines like IL‑6 and TNF‑α. Chronic inflammation is a well‑known driver of pancreatic neoplasia.
- Immune Evasion: High cortisol levels shrink the activity of cytotoxic T‑cells and natural killer cells, allowing early tumor clones to escape detection.
- Metabolic Reprogramming: Adrenaline activates β‑adrenergic receptors on pancreatic cells, boosting glycolysis (the Warburg effect) and providing fuel for rapid growth.
- KRAS Mutation Synergy: The majority (≈90%) of pancreatic cancers harbor activating KRAS mutations. Stress‑induced ROS (reactive oxygen species) can further entrench KRAS signaling, pushing cells toward malignant transformation.
These mechanisms are not isolated; they intersect, creating a feedback loop where stress hormones perpetuate a hostile microenvironment that nurtures cancer.
Comparing Cortisol and Adrenaline Effects
| Aspect | Cortisol | Adrenaline |
|---|---|---|
| Primary source | Adrenal cortex | Adrenal medulla & sympathetic nerves |
| Receptor type | Glucocorticoid receptor (GR) | β‑adrenergic receptor (β‑AR) |
| Impact on DNA repair | Inhibits p53‑dependent repair | Indirect via oxidative stress |
| Inflammatory signaling | Modulates NF‑κB (both up & down) | Activates NF‑κB and MAPK pathways |
| Metabolic effect | Promotes gluconeogenesis | Enhances glycolysis and lactate production |
| Immune modulation | Suppresses T‑cell activity | Reduces NK‑cell cytotoxicity |
Epidemiological Evidence Linking Stress to Pancreatic Cancer
Large‑scale cohort studies from the United States, Europe, and Asia reveal consistent patterns:
- Occupational stress: A 2022 meta‑analysis of 12 prospective studies found a 27% higher pancreatic cancer risk among individuals reporting high job strain compared to low strain.
- Psychological distress: The EPIC‑Heidelberg cohort (n≈500,000) showed that participants with the highest scores on the Perceived Stress Scale had a hazard ratio of 1.32 for pancreatic cancer, even after adjusting for smoking, alcohol, and BMI.
- Life‑event burden: A Taiwanese case‑control study linked the experience of ≥3 major stressful events in the past year to a 1.5‑fold increase in pancreatic cancer odds.
These findings hold after controlling for classic risk factors, suggesting an independent contribution of chronic stress.

Managing Stress to Lower Pancreatic Cancer Risk
While you can’t erase past stress, you can reshape how your body handles it. Below are evidence‑backed tactics that directly target the hormonal pathways described earlier.
- Mind‑body practices: Randomized trials show that an 8‑week mindfulness‑based stress reduction (MBSR) program cuts salivary cortisol by ~15% and improves immune markers (↑ NK‑cell activity).
- Physical activity: Moderate‑intensity aerobic exercise (150min/week) lowers basal cortisol and adrenaline, while also reducing insulin resistance - a known pancreatic cancer driver.
- Sleep hygiene: Restoring a regular 7-9‑hour sleep pattern normalizes the HPA axis. One study found that sleep‑restricted volunteers had a 30% spike in plasma cortisol.
- Pharmacologic modulation: β‑blockers (e.g., propranolol) have shown promise in preclinical mouse models, slowing pancreatic tumor growth by 40% via β‑AR blockade.
- Nutrition: Diets rich in omega‑3 fatty acids (found in fatty fish) attenuate inflammation and may blunt cortisol‑induced immune suppression.
Practical Stress‑Reduction Checklist for Pancreatic Health
- Schedule a 10‑minute breathing exercise twice daily (inhale 4s, hold 4s, exhale 6s).
- Walk briskly for 30minutes at least three times a week.
- Turn off screens 1hour before bedtime; aim for consistent sleep‑wake times.
- Eat two servings of oily fish per week; add a handful of walnuts as a snack.
- If you have high blood pressure or heart issues, discuss β‑blocker therapy with your doctor.
- Keep a stress diary: note triggers, intensity (1‑10), and coping actions - patterns help you intervene early.
Implementing these steps doesn’t guarantee cancer prevention, but it tackles the biological pathways that link chronic stress to pancreatic tumor development.
Research Gaps and Future Directions
Even with mounting evidence, several questions linger:
- Which specific glucocorticoid‑receptor polymorphisms heighten pancreatic susceptibility?
- Can long‑term β‑blocker use reduce incidence in high‑risk populations (e.g., familial pancreatic cancer carriers)?
- How do stress‑induced microbiome shifts influence pancreatic inflammation?
- What is the optimal timing for stress‑reduction interventions relative to cancer diagnosis?
Answering these will require interdisciplinary trials that combine oncology, endocrinology, and behavioral medicine.
Bottom Line
Stress isn’t just a feeling; it’s a hormonal cascade that can push a normal pancreas toward malignancy and accelerate an existing tumor. By understanding the science-how cortisol, adrenaline, inflammation, and immune suppression intertwine-you gain concrete levers to act on. Whether through mindfulness, movement, sleep, or, where appropriate, medication, you can blunt the stress‑cancer link and give your pancreas a better chance at staying healthy.
Frequently Asked Questions
Does occasional stress increase pancreatic cancer risk?
Occasional, short‑lived stress spikes cortisol and adrenaline briefly, which the body can recover from. It’s chronic, unrelenting stress-lasting weeks to months-that creates the hormonal environment linked to tumor initiation and progression.
Can stress‑reduction therapies improve outcomes after a pancreatic cancer diagnosis?
Early studies suggest that patients who engage in mindfulness, yoga, or counseling have better quality‑of‑life scores and may tolerate chemotherapy longer. Direct survival benefits are still under investigation, but reducing stress certainly helps the immune system stay more active.
Are there medications that block the harmful effects of stress hormones on pancreatic cancer?
Beta‑blockers, which inhibit adrenaline’s action on β‑adrenergic receptors, have shown promise in animal models and some retrospective human studies. However, they’re not a standard cancer therapy yet; discuss with your oncologist before adding any new drug.
How does sleep affect stress hormones related to cancer?
Poor sleep or fragmented sleep raises nighttime cortisol and blunts the normal dip in adrenaline. Over time, this disrupts the HPA axis, leading to the same pro‑tumor environment described earlier. Prioritizing 7‑9 hours of restorative sleep helps keep those hormones in check.
Is there a genetic test for stress‑related pancreatic cancer risk?
Currently, no single test predicts risk based on stress alone. Genetic panels can identify high‑risk mutations (e.g., BRCA2, CDKN2A), but the interaction between those genes and chronic stress is still being studied.




Comments
Natala Storczyk
October 17, 2025
When the relentless grind of daily life pushes your mind to the brink, the body answers with a storm of cortisol and adrenaline that never seems to calm down!!! It’s like living inside a pressure cooker that never releases steam, and every cell in your pancreas feels the heat.
Scientists have mapped exactly how this hormonal overload can break DNA strands, mute the guardians of the genome, and whisper to rogue cells that it’s safe to multiply.
The HPA axis, that ancient command center, stays stuck in overdrive, flooding your bloodstream with the very chemicals that were meant to protect you in short bursts.
Chronic stress doesn’t just make you tired; it rewires the immune system, shrinking the army of cytotoxic T‑cells and natural killers that would normally hunt emerging tumors.
And let’s not forget the metabolic shift – adrenaline fuels a Warburg‑like frenzy, turning pancreatic cells into power‑hungry beasts that devour glucose and grow unchecked.
All of this creates a perfect storm for KRAS‑mutated cells, the hallmark of most pancreatic cancers, to seize the advantage and turn malignant.
Epidemiological data from dozens of cohorts scream the same message: high‑stress jobs, relentless anxiety, and a life without proper recovery boost your odds of pancreatic cancer by a staggering 25‑30%!!!
But there is hope – the same pathways that wreak havoc can be tamed with mindfulness, regular exercise, and even beta‑blockers that block adrenaline’s malicious signals.
Imagine a daily ritual of deep breaths, a brisk walk, and a solid night’s sleep that together reset the HPA axis, lower cortisol, and give your immune system a fighting chance.
Clinical trials already show that eight weeks of mindfulness can slash salivary cortisol by fifteen percent and revive NK‑cell activity.
Physical activity, even at moderate intensity, cuts basal cortisol and improves insulin sensitivity, tackling another pillar of pancreatic tumor growth.
Sleep hygiene is another low‑cost weapon: consistent 7‑9‑hour cycles prevent the nocturnal cortisol spikes that keep the tumor micro‑environment hostile.
For those with cardiovascular risk, discussing beta‑blocker therapy with a doctor could add a pharmacologic shield against adrenaline’s tumor‑promoting effects.
In short, chronic stress is not a harmless mood‑swing; it is a biochemical engine that can power pancreatic cancer from its very inception to its deadliest stages. Take control, and you may just turn off that engine before it burns you out.
Sarah Hanson
October 18, 2025
Thank you for the thorough overview. This summary concisely outlines actionable steps without oversimplifying the science.
Nhasala Joshi
October 20, 2025
Wow, the data you presented is practically a blueprint for the hidden elite to keep us in chronic fear!!! The stress‑hormone loop is a covert weapon used by a hidden agenda to suppress the masses.🔬🧬 The way cortisol sabotages p53 is like a silent assassin, and they don’t want us to know it 😱. Let’s stay vigilant, question the mainstream narrative, and push for transparent research on stress‑blocking meds! 💥
kendra mukhia
October 21, 2025
Honestly, the whole “stress causes cancer” angle has been blown out of proportion by sensationalists. The mechanisms you listed are real, but most people will never reach that level of chronic hormonal overload unless they *choose* a toxic lifestyle. It’s a wake‑up call to stop making excuses and start taking responsibility for daily habits. If you’re not willing to change, the science will just confirm what you already know.
Bethany Torkelson
October 22, 2025
I appreciate the practical checklist – it’s exactly what patients need to feel empowered. Stress isn’t a fate, it’s a modifiable risk factor. Simple breathing and regular walks can actually shift hormone levels. Keep spreading this knowledge.
Grace Hada
October 23, 2025
The checklist is solid, but remember that philosophical acceptance of stress also matters. One must confront the existential roots of anxiety, not just the symptoms. Only then can the interventions be truly effective.
alex montana
October 24, 2025
??Wow!!! The link between cortisol and DNA damage is pretty intense??
Don’t overlook the power of beta‑blockers – they could be a game‑changer.
Wyatt Schwindt
October 25, 2025
Great summary. It’s good to see science and lifestyle guidance together.
Lyle Mills
October 27, 2025
From a mechanistic standpoint, integrating stress‑reduction with metabolic control addresses both endocrine and oncogenic pathways. The synergy between reduced cortisol and improved insulin sensitivity is especially relevant for KRAS‑driven tumors.
Barbara Grzegorzewska
October 28, 2025
Honestly, this article reads like a high‑brow lecture – but the point is clear: stress is a silent architect of pancreatic doom. The science is solid, the recommendations are doable, and the tone is just a tad pretentious. Still, kudos for not over‑simplifying. Keep the nuance, but maybe drop the jargon a notch for the average reader.
Nis Hansen
October 29, 2025
Indeed, the interplay of neuroendocrine stress signals and tumor micro‑environment is a fascinating frontier. By marrying behavioral interventions with pharmacologic targets, we can potentially rewire the HPA axis toward resilience. Let’s champion interdisciplinary trials that move beyond siloed approaches.
Fabian Märkl
October 30, 2025
Love how you broke this down – very helpful! 👍😊
Avril Harrison
October 31, 2025
Nice read, especially the part about breathing exercises. I might try that during my morning tea.
nitish sharma
November 1, 2025
Thank you for presenting the evidence so clearly. I encourage everyone to adopt at least one of the suggested stress‑reduction practices.
Write a comment