What Is Deep Brain Stimulation for Parkinson’s?
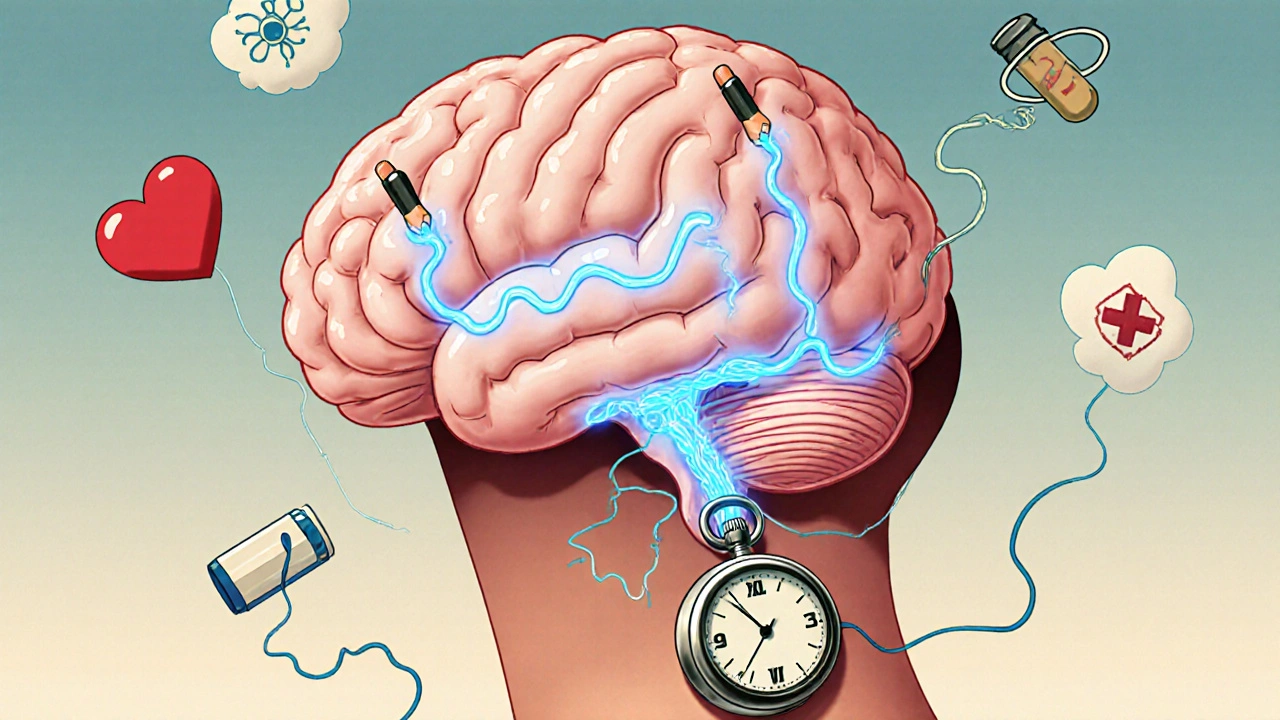
Deep Brain Stimulation, or DBS, is a surgical treatment for Parkinson’s disease that uses implanted electrodes to send electrical pulses to specific areas of the brain. It doesn’t cure Parkinson’s, but it can dramatically reduce the worst motor symptoms-like tremors, stiffness, and freezing-that don’t respond well to medication anymore. Think of it like a pacemaker for your brain: instead of regulating heartbeat, it regulates abnormal brain signals causing movement problems.
DBS became widely used after the FDA approved it for Parkinson’s in 2002. Since then, the technology has evolved. Modern systems like Medtronic’s Percept™ PC and Boston Scientific’s Vercise™ Genus™ can not only deliver stimulation but also record brain activity in real time. This lets doctors adjust settings based on what the brain is actually doing, not just what the patient reports. These systems use rechargeable batteries that last 9 to 15 years and connect wirelessly to smartphones or tablets for remote programming.
How DBS Works: Targets, Settings, and Technology
The surgery involves placing thin electrodes (about the width of a pencil lead) into two key brain areas: the subthalamic nucleus (STN) or the globus pallidus interna (GPi). Both targets help with movement control, but they affect patients differently.
STN stimulation tends to let patients reduce their levodopa doses by 30-50%, which cuts down on drug-induced dyskinesias. But it can sometimes cause mood or speech side effects. GPi stimulation doesn’t reduce medication as much, but it’s better at controlling dyskinesias directly and is less likely to affect thinking or emotions. Most surgeons choose STN for younger patients with strong levodopa response and GPi for older patients or those with existing cognitive concerns.
The electrical pulses are delivered at 60-185 Hz, with pulse widths between 60 and 450 microseconds. Voltages range from 0.5 to 10.5 volts. These settings are fine-tuned over months, not days. The device is powered by an implantable pulse generator (IPG), usually placed under the skin near the collarbone or abdomen. The whole system-electrodes, wires, and IPG-is designed to last for years, but battery replacement or lead revisions may be needed.
Who Is a Good Candidate for DBS?
Not everyone with Parkinson’s qualifies. The most important factor is response to levodopa. If your symptoms improve significantly when you take your medication, you’re likely a good candidate. Doctors measure this using the Unified Parkinson’s Disease Rating Scale (UPDRS). A 30% or better improvement in motor scores after taking levodopa is the minimum threshold.
You also need to have had Parkinson’s for at least five years. This isn’t arbitrary-it’s because early-stage patients often respond well to meds alone, and later-stage patients may have too many non-motor symptoms that DBS won’t fix. Patients with atypical parkinsonism-like progressive supranuclear palsy or multiple system atrophy-usually don’t benefit. Their symptoms don’t respond to levodopa, so DBS won’t either.
Cognitive health matters too. If your memory or thinking is already impaired (MMSE score below 24 or MoCA below 21), DBS can make things worse. Depression and anxiety need to be managed before surgery, as they can affect recovery and satisfaction. A neuropsychological evaluation is standard before approval.
What DBS Can and Can’t Do
DBS is excellent for motor symptoms that respond to levodopa: tremors, rigidity, bradykinesia, and medication-induced dyskinesias. In the landmark EARLYSTIM trial, patients who got DBS early saw a 23-point improvement in quality of life scores on the PDQ-39 scale-nearly double the improvement seen with medication alone.
But it doesn’t help everything. Gait freezing, balance issues, and speech problems improve only slightly-about 20-30%. Swallowing difficulties, constipation, sleep problems, and depression usually don’t get better. Some patients expect DBS to stop the disease from progressing. It doesn’t. It only masks the symptoms that respond to levodopa.
Real-world stories reflect this. One patient on the Parkinson’s Foundation Forum said his OFF time dropped from six hours a day to one. Another on Reddit admitted his tremors vanished but now he struggles to plan simple tasks. Managing expectations is half the battle.
The Evaluation Process: What to Expect Before Surgery
Getting approved for DBS isn’t quick. It usually takes 3 to 6 months. First, a movement disorder neurologist confirms the diagnosis and checks levodopa response. Then comes neuropsychological testing-4 to 6 hours of memory, attention, and executive function tests. A high-resolution 3T MRI is done to map the brain and plan electrode placement.
After that, a multidisciplinary team reviews everything: neurologist, neurosurgeon, neuropsychologist, and sometimes a psychiatrist or speech therapist. They decide whether you’re a candidate, which target (STN or GPi) is best, and whether one or both sides of the brain should be stimulated.
Insurance approval is another hurdle. Medicare and most private insurers cover DBS for Parkinson’s, but they require proof that you’ve tried and failed to get stable control with medication. That means documenting at least 6 months of optimized drug regimens, often with detailed logs of symptom fluctuations.
Outcomes: Success Rates and Complications
When done right, DBS works. About 70-80% of properly selected patients get major motor improvement. In the EARLYSTIM trial, 78% reported meaningful gains in daily life. Many regain the ability to walk without freezing, dress themselves, or hold a cup without shaking.
But complications happen. About 1-3% of patients have a brain bleed during surgery. Around 5-15% develop hardware issues-loose wires, infections, or broken leads-that need revision surgery. Battery replacements are common with older non-rechargeable devices, happening every 3-5 years. Newer rechargeable systems reduce this need, but patients still need to charge them regularly.
Cognitive side effects are subtle but real. Word-finding trouble, slower thinking, or reduced motivation occur in 10-20% of patients. These aren’t always permanent, but they can require speech therapy or adjustments in stimulation settings. That’s why follow-up visits are crucial. The first year often involves 6-12 monthly programming sessions to fine-tune the device.
How DBS Compares to Other Treatments
DBS isn’t the only option. Focused ultrasound (Exablate Neuro) is non-invasive and FDA-approved for tremor-dominant Parkinson’s. But it only treats one side of the brain and doesn’t help with other motor symptoms like slowness or stiffness. It’s also not reversible.
Lesioning procedures like pallidotomy or thalamotomy destroy small parts of the brain to stop abnormal signals. They work well, but the damage is permanent. If something goes wrong, you can’t undo it. DBS is adjustable and reversible-you can turn it off or remove it if needed.
Compared to medication alone, DBS wins for motor complications. The EARLYSTIM trial showed DBS patients had 60-80% fewer motor fluctuations and 80% less dyskinesia. Medication alone can’t match that level of control long-term.
Why So Few People Get DBS
Despite its benefits, only 1-5% of eligible Parkinson’s patients get DBS. Why? Many are never referred. Doctors sometimes assume patients are too old, too sick, or too far along. Others don’t know about the criteria. Patients themselves often fear brain surgery or think it’s a last resort.
But the data says otherwise. The EARLYSTIM trial showed that patients who got DBS earlier-after just 4 years of disease-had better long-term outcomes than those who waited. DBS isn’t a final step. It’s a tool to preserve quality of life during the middle stages of Parkinson’s.
Center experience matters too. Hospitals that do more than 50 DBS procedures a year have 20% fewer complications. If you’re considering DBS, look for a center with a dedicated movement disorders team, not just a neurosurgeon working alone.
What’s Next for DBS?
The future of DBS is personalization. New systems like Medtronic’s Percept™ PC can sense brain signals in real time and adjust stimulation automatically. The INTREPID trial showed this closed-loop approach improved symptom control by 27% over traditional DBS.
Researchers are exploring whether DBS can help with non-motor symptoms like depression or apathy. Early studies suggest it might, especially when targeting different brain areas. Genetic testing is also emerging-people with LRRK2 gene mutations respond better to DBS, which could help predict outcomes.
One of the biggest shifts is moving toward earlier intervention. The EARLYSTIM-2 trial is testing DBS in patients with only 3 years of Parkinson’s. If results are positive, the standard of care could change completely.
Final Thoughts: Is DBS Right for You?
If you’ve been on levodopa for five or more years and still struggle with OFF periods, dyskinesias, or tremors that meds can’t control, DBS could be life-changing. But it’s not a magic fix. It requires commitment-to evaluations, programming visits, and understanding its limits.
Start by talking to a movement disorder specialist. Ask: "How much do my symptoms improve with levodopa?" and "Have my thinking or mood changed recently?" If your answers point to strong medication response and no major cognitive issues, you’re likely a good candidate.
Don’t wait until you’re too disabled. DBS works best when you’re still active enough to benefit from it. The goal isn’t to return to how you were 20 years ago. It’s to get back to who you are now-without being held back by your symptoms.
Can DBS cure Parkinson’s disease?
No, DBS does not cure Parkinson’s. It only treats the motor symptoms that respond to levodopa, such as tremors, stiffness, and dyskinesias. It does not stop the disease from progressing or improve non-motor symptoms like memory loss, constipation, or sleep problems.
How long does it take to see results after DBS surgery?
Improvement in motor symptoms often happens right after the device is turned on, usually 2-4 weeks after surgery. But full optimization takes 6-12 months of programming visits. Settings need to be adjusted as your body heals and your medication schedule stabilizes.
Is DBS safe for older patients?
Age alone doesn’t disqualify someone. Patients in their 70s and even 80s can benefit if they’re otherwise healthy, have strong levodopa response, and no significant cognitive decline. The key is overall health, not age. Many older patients report improved independence and reduced fall risk after DBS.
What happens if the battery runs out?
If the battery dies, stimulation stops and symptoms return. Rechargeable systems last 9-15 years and need weekly charging. Non-rechargeable batteries last 3-5 years and require minor surgery to replace. Most centers monitor battery status remotely and alert patients before it’s time to replace.
Can I have an MRI after DBS surgery?
Yes, but only with specific MRI machines and settings. Most modern DBS systems are MRI-conditional, meaning you can have a 1.5T or 3T MRI if the device is turned off and proper safety protocols are followed. Always inform your radiology team you have a DBS implant before any scan.
Will I still need to take Parkinson’s medication after DBS?
Yes, most patients still need medication, but usually at lower doses. DBS reduces the need for levodopa by 30-50% on average. This helps cut down on side effects like dyskinesias. Some patients can reduce their pills significantly, but stopping all medication is rare and not recommended.
What are the biggest risks of DBS surgery?
The main risks are brain bleeding (1-3%), infection (2-5%), and hardware problems like broken wires or misplaced leads (5-15%). Cognitive side effects, such as word-finding trouble or reduced motivation, occur in 10-20% of patients. These are often manageable with programming adjustments or therapy.
How do I find a good DBS center?
Look for centers that perform more than 50 DBS procedures per year and have a dedicated multidisciplinary team including neurologists, neurosurgeons, and neuropsychologists. Academic medical centers often have the most experience. Ask if they use modern systems with sensing capabilities and whether they offer remote programming support.





Comments
Tom Shepherd
November 27, 2025
DBS sounds like sci-fi but it's real and it works. I've seen my uncle go from barely walking to playing with his grandkids again. No magic cure but damn if it isn't close.
Jauregui Goudy
November 27, 2025
Let me tell you something - if you're still on meds and your tremors are winning, you're not being weak, you're being patient. DBS isn't a last resort, it's a reset button. I wish someone told me that five years ago. The programming visits suck but the payoff? Worth every minute.
shawn monroe
November 27, 2025
From a neuroengineering standpoint, the closed-loop systems like Percept PC are game-changers. The adaptive stimulation algorithms leverage local field potential (LFP) biomarkers to dynamically modulate beta-band oscillations in the STN, effectively decoupling pathological synchrony. This isn't just palliative - it's neuromodulatory precision medicine. The EARLYSTIM trial's PDQ-39 data? That's not anecdotal, that's effect size Cohen's d > 0.8. We're talking clinically significant quality-of-life shifts.
Kaleigh Scroger
November 29, 2025
I've been doing this for 12 years as a movement disorder nurse and let me tell you the biggest mistake people make is waiting until they're stuck in a chair. If you're still driving, still working, still cooking dinner - that's your window. The surgery isn't the hard part, it's the months of programming. My patients who got it at year 4-5? They're the ones still hiking. The ones who waited until they couldn't stand? They're the ones who regret it. Don't wait for the worst day to act. The brain adapts better when it's still flexible.
And yes, you'll still need meds. DBS doesn't erase levodopa, it just lets you breathe again. Lower dose, fewer dyskinesias, better sleep. I had a patient cut her pills from 12 to 4 a day. That's not a side effect, that's liberation.
And don't let anyone tell you age is a barrier. I had an 82-year-old woman get it last year. She was terrified. Now she's teaching yoga to other patients. It's not about age, it's about brain health and response. If levodopa works, you're a candidate. Period.
The battery thing? Rechargeable ones last a decade. You charge it like your phone. Once a week. Five minutes. That's it. The fear of surgery is real but the fear of being trapped in your own body? That's worse.
And yes, you'll still have bad days. DBS doesn't fix freezing or swallowing. But it gives you back the good days. And that's everything.
Elizabeth Choi
November 30, 2025
78% success rate? That's statistically significant but practically meaningless if you're in the 22%. Also, the EARLYSTIM trial had strict exclusion criteria - no cognitive decline, no depression, no comorbidities. Real-world patients? Most don't fit that profile. The data looks great on paper but the clinic is messy. And don't get me started on the cost of follow-ups. Insurance covers the surgery but not the 12 programming visits. That's $15k out of pocket for most.
Emma Dovener
November 30, 2025
I'm a speech therapist who works with DBS patients. The word-finding issues are real but often overlooked. We do a lot of semantic fluency exercises and pacing drills. It's not about stopping stimulation - it's about retraining the brain. A lot of patients think it's permanent but with therapy, 80% improve within 6 months. Don't panic if you stumble on words. Just keep talking. Your brain is rewiring.
Sue Haskett
December 1, 2025
PLEASE, PLEASE, PLEASE if you're considering this, find a center that does at least 50 cases a year. Seriously. I know someone who had her lead placed in the wrong spot because the surgeon only did this once a month. She had to have revision surgery. And now she's terrified of even going to the doctor. Don't let that be you. Ask for their annual volume. Ask for their complication rates. Ask for their neuropsych team. This isn't a one-surgeon show. It's a team sport. And your brain deserves the best team.
Leo Adi
December 1, 2025
In India, we don't talk about this much. But my uncle had it done in Bangalore last year. He was skeptical. Now he walks to the temple every morning without help. The cost? Less than a year of his meds. The real barrier here isn't money, it's silence. We don't ask. We don't research. We just suffer. This isn't just for the West. It's for anyone who still has a spark left in them.
archana das
December 2, 2025
Life is not about being cured. It's about being free. DBS doesn't fix Parkinson's. But it gives you back your hands. Your voice. Your dignity. I used to cry when I couldn't button my shirt. Now I make chai for my grandchildren every morning. That's not science. That's grace.
Emma louise
December 3, 2025
So let me get this straight - you're going to drill holes in your skull and stick wires in your brain because you don't want to take your pills? That's not medicine, that's tech bro fantasy. Next they'll be selling brain chips to fix bad marriages. Wake up. Parkinson's is part of aging. Stop trying to hack death.
Write a comment