Why do patients keep taking expensive drugs when cheaper, equally effective options are right there? It’s not about ignorance. It’s not about laziness. It’s about how the human brain actually works - and that’s where behavioral economics comes in.
People don’t choose drugs like robots
Traditional medicine assumes patients are rational actors. If Drug B costs 30% less than Drug A and works just as well, they’ll switch. Simple, right? But in real life, that rarely happens. A 2022 study found that 68% of patients stick with their current medication - even when a cheaper alternative is available. Why? Because people don’t weigh costs and benefits like accountants. They react to fear, habits, and emotions.Take loss aversion. It’s the idea that losing something feels worse than gaining something of equal value. When a patient has been on a drug for months, switching feels like losing control, even if the new drug is better. They don’t think, "This is cheaper." They think, "What if this doesn’t work? What if I feel worse?" That fear is stronger than any price tag.
And then there’s confirmation bias. Patients often believe more expensive drugs are better. A 2022 study showed prescription drug prices rose 47% faster than general inflation over the last decade - and patients didn’t question it. They assumed higher cost = higher quality. Even when doctors explained otherwise, many stuck with the pricier option.
The hidden forces shaping drug choices
Behavioral economics uncovers the invisible forces driving these decisions. Here are the big ones:- Present bias: People choose immediate comfort over long-term health. Thirty-three percent of prescriptions are never filled, even when the patient knows skipping doses could lead to serious complications. They think, "I feel fine today," and push it off.
- Complexity overload: Patients on five or more medications have adherence rates 23.7% lower than those on just one. Every extra pill, every different time of day, every new instruction adds mental friction. The brain shuts down.
- Social norms: People follow the crowd. One HIV clinic posted signs showing how many patients were taking their meds on time. Adherence jumped 22.3%. No one wanted to be the outlier.
- Framing: Saying a vaccine is "95% effective" gets more takers than saying it has a "5% failure rate." The same fact, two totally different reactions.
These aren’t quirks. They’re predictable patterns. And once you see them, you can design better systems.
How doctors and pharmacies are fixing this
Some health systems are no longer just giving advice. They’re redesigning choices.At one hospital, doctors noticed patients weren’t switching to generic statins during drug shortages. So they changed the default setting in the electronic health record. Instead of the brand-name drug appearing first, the generic was pre-selected. Within months, appropriate substitutions jumped by 37.8%.
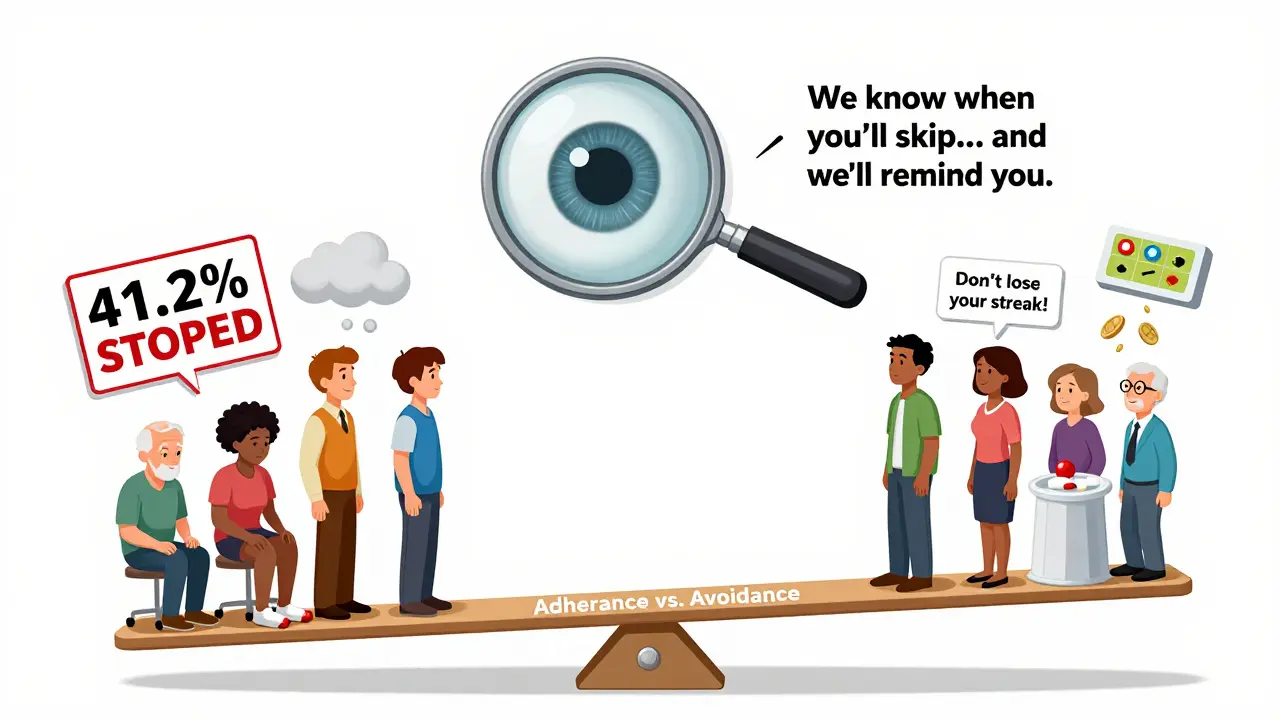
Another program used SMS messages. Instead of saying, "Take your medication," they wrote, "Don’t lose your streak!" - tapping into loss aversion. Adherence improved by 19.7%. Simple words. Big impact.
Some insurers now offer rebates for consistent pill-taking. Patients earn money back if they take their meds for 90 days straight. In a 2021 NEJM study, this approach boosted statin persistence by 23.8% compared to no incentive.
These aren’t gimmicks. They’re behavioral nudges - small changes in how choices are presented that lead to big shifts in behavior. And they work better than pamphlets, lectures, or reminders that say "Take your pills."

Why education alone fails
For decades, the go-to fix was patient education. Give them brochures. Hold workshops. Explain side effects. But here’s the truth: those programs typically improve adherence by only 5-8%. Behavioral interventions? They boost it by 14-28%.Why the gap? Because knowledge doesn’t change behavior. You know smoking is bad. You know sitting too long is unhealthy. But you still do it. The same applies to meds. A patient might fully understand that their blood pressure drug needs to be taken daily - but if they forget, feel overwhelmed, or fear side effects, they’ll skip it anyway.
Behavioral economics doesn’t assume people are irrational. It assumes they’re human. And humans need help making good choices when they’re tired, stressed, or confused.
Barriers no one talks about
Not all patients respond the same way. Some barriers are deeper:- Polypharmacy: Each extra medication cuts adherence by 8.3%. Five pills? That’s a 41.5% drop in likelihood of taking them all.
- Asymptomatic conditions: If you don’t feel sick, why take a pill? Patients with high cholesterol or early-stage diabetes have adherence rates 32.7% lower than those with painful symptoms.
- Negative beliefs: 41.2% of people stop their meds because they believe the drug is unnecessary, harmful, or just "not for them."
- Mental health: Depression slashes adherence by 28.4%. Anxiety makes it worse. These aren’t just side effects - they’re barriers to treatment.
One-size-fits-all programs fail here. A patient with depression won’t respond to a text reminder. They need someone checking in. A person with complex meds needs simplified packaging. Tailoring matters.
The cost of getting it wrong
This isn’t just about convenience. It’s about lives.Medication non-adherence costs the U.S. healthcare system $289 billion a year. That’s more than diabetes, heart disease, and cancer combined. And it leads to 125,000 avoidable deaths annually.
Pharmaceutical companies are taking notice. McKinsey reported that firms using behavioral economics in patient support programs saw 17.3% higher persistence and 22.8% fewer discontinuations. That’s not just good for patients - it’s good for business.
The FDA now requires drug sponsors to evaluate how dosing schedules and pill size affect patient decisions. Medicare Part D plans must include at least two behavioral interventions for high-risk patients. This isn’t a trend - it’s becoming standard.
What’s next?
The future is personalization. Researchers are training AI to predict which patients will respond to which nudges. Maybe one person needs a text reminder. Another needs a home visit. Another needs their pill bottle to beep when it’s time.Early pilot studies show machine learning can boost intervention effectiveness by 42.3%. Imagine a system that knows you’re more likely to skip meds on weekends - and sends a voice message on Friday afternoon: "Your heart needs you tomorrow. Don’t let it down."
And as biosimilars enter the market, behavioral nudges are helping patients switch from expensive brand-name drugs. One study showed a 29.4% increase in adoption when patients were given clear, simple comparisons - not just price tags, but stories: "Other patients like you switched and saved $1,200 a year without losing control of their condition."
What patients can do
You don’t need a PhD to beat these biases. Here’s what helps:- Ask your doctor: "Is there a cheaper option that works just as well?" Don’t assume the first drug they suggest is the only one.
- Use a pill organizer - even a simple one. It cuts mental load.
- Set a daily alarm. Not just "take pill" - make it personal: "I’m doing this for my kids."
- If you’re feeling overwhelmed, say so. Your doctor can simplify your regimen.
- Don’t judge yourself for skipping a dose. Just restart. Guilt makes it worse.
Behavioral economics doesn’t blame patients. It fixes the system. And that’s the real breakthrough.
Why do patients keep taking expensive drugs even when cheaper ones are available?
Patients don’t always choose based on price because human decisions are shaped by emotions, habits, and cognitive biases. Loss aversion makes them fear losing what they’re used to, confirmation bias leads them to believe more expensive drugs are better, and present bias makes them prioritize immediate comfort over long-term health - even when they know better.
How does loss aversion affect medication adherence?
Loss aversion means people feel the pain of losing something more strongly than the pleasure of gaining something equal. When patients switch medications, they fear losing the perceived benefits of their current drug - even if the new one is equally effective. This fear often overrides cost savings, leading many to stick with pricier options.
What’s the difference between patient education and behavioral nudges?
Patient education gives information - like pamphlets or lectures - but rarely changes behavior. Behavioral nudges change how choices are presented to make the right choice easier. Examples include defaulting to generic drugs in prescriptions, sending text messages that say "Don’t lose your streak!" or offering rebates for consistent use. These work because they align with how people actually think, not how they should think.
Can behavioral economics help with chronic conditions like diabetes or high blood pressure?
Yes - and it’s already being used successfully. Diabetes has the highest adoption of behavioral interventions (47.8% of programs) because regular dosing creates clear opportunities for nudges. Programs using defaults, reminders, and incentives have boosted adherence by up to 28%. These approaches work better than education alone because they reduce the mental effort needed to stay on track.
Why don’t more doctors use behavioral economics?
Many doctors haven’t been trained in it, and integrating these strategies into busy clinics takes time and tech. Electronic health record systems often don’t support behavioral defaults. Staff training requires about 12.7 hours per clinician, and 78.3% of institutions report compatibility issues. But adoption is growing fast - especially in large hospitals and with payers who see the cost savings.
Are behavioral interventions ethical?
Some critics worry about manipulating patients. But behavioral nudges preserve freedom - patients can still choose to ignore them. Unlike forced mandates, nudges gently guide without restricting options. Experts like Dr. Aaron Kesselheim argue they’re ethical because they respect autonomy while making better choices easier. The goal isn’t control - it’s support.
How much does it cost to implement behavioral interventions?
Costs vary. Basic SMS reminders cost about $8.25 per patient per month. Smart pill bottles with feedback cost $47.50. But the savings are huge: non-adherence costs the U.S. $289 billion yearly. Programs that improve adherence by just 10% can pay for themselves many times over through reduced hospitalizations and ER visits.
Do these strategies work for mental health conditions like depression?
They’re less effective - adherence drops by 28.4% in patients with depression. Standard nudges like texts or reminders often don’t reach people who feel too overwhelmed to act. Success requires combining behavioral tools with mental health support: home visits, peer coaching, or simplified regimens. One-size-fits-all doesn’t work here - personalized care is essential.






Comments
Greg Quinn
December 29, 2025
It’s wild how we treat meds like they’re just data points when they’re really emotional anchors. You’re not just taking a pill-you’re clinging to a version of yourself that feels in control. That’s why defaults work: they let you keep that illusion without the mental tax. We’re not lazy. We’re just trying to survive the noise.
And honestly? The fact that we’ve built a whole system around punishing people for forgetting pills while ignoring why they forget… that’s the real tragedy.
Lisa Dore
December 30, 2025
I love how this post flips the script-no blame, just understanding. My grandma took her blood pressure med for years but skipped it every weekend because she said, 'I don’t feel sick on Saturday.' We thought she was being stubborn. Turns out, she was just human.
Now we use a little sticker chart with her grandkids’ drawings. She doesn’t want to let them down. No lecture needed. Just connection. Small things, huge impact.
Sharleen Luciano
December 31, 2025
Oh please. This is just behavioral economics dressed up as virtue signaling. You’re telling me we need AI and SMS nudges because patients are too stupid to read a prescription label? Let’s not confuse systemic failures with biological incompetence.
People don’t take meds because they’re lazy, irresponsible, or emotionally fragile-they’re doing it because the system is rigged. Pharma sets prices, insurers dictate formularies, and doctors are too busy to explain anything. Stop pathologizing patients and fix the damn architecture.
And don’t get me started on ‘loss aversion.’ That’s just a fancy word for ‘people don’t trust doctors anymore.’ And honestly? Fair.
Jim Rice
December 31, 2025
You people are ridiculous. You think a text saying ‘Don’t lose your streak!’ is going to fix a $289 billion problem? That’s like putting a bandaid on a severed artery.
Real solution? Make generics the only option. Ban brand-name prescriptions unless there’s a clinical reason. No defaults. No nudges. Just eliminate the choice. People complain about being ‘manipulated’-fine. Let them complain while they’re not in the ER because they skipped their statin.
And stop pretending this is about empathy. It’s about cost control disguised as psychology.
Henriette Barrows
January 1, 2026
I’ve seen this firsthand with my mom. She had three meds for three different things, all at different times. She’d get overwhelmed and just… stop. Not because she didn’t care. Because her brain literally couldn’t handle it.
Then her pharmacist gave her a pill organizer with color-coded sections and a simple note: ‘You’ve got this.’ That’s it. No lectures. No apps. Just clarity.
She started taking everything again. Not because she was ‘nudged.’ Because someone finally made it feel possible.
Teresa Rodriguez leon
January 3, 2026
It’s not about behavior. It’s about poverty. If you’re working two jobs, living paycheck to paycheck, and your kid has a fever, you’re not thinking about your cholesterol. You’re thinking about whether the lights will stay on.
Behavioral nudges are a luxury for people who have the mental bandwidth to care. For the rest of us? We need cheaper meds. Full stop.
Manan Pandya
January 4, 2026
This is beautifully articulated. In India, we see similar patterns-patients stop antihypertensives because they feel fine, or avoid insulin due to stigma. But what’s missing here is cultural context. In collectivist societies, family involvement often improves adherence more than any nudge.
One clinic in Jaipur trains family members as ‘medication ambassadors.’ They don’t just remind-they sit with the patient, eat with them, normalize the routine. The result? 34% higher persistence.
Human connection is the original nudge.
Aliza Efraimov
January 5, 2026
Let me tell you about my cousin. Diagnosed with Type 2 diabetes. Doctor gave him a 10-page pamphlet. He threw it out.
Then his sister started texting him every morning: ‘Bro, you’re the reason Mom sleeps easy. Don’t make me worry.’
He started taking his meds. Not because of science. Because he loved her. And that’s the missing piece: love, not logic.
Why are we spending millions on AI when we could just teach doctors to say, ‘Who’s counting on you?’
Nisha Marwaha
January 6, 2026
From a public health implementation science perspective, the efficacy of behavioral interventions is contingent upon fidelity of delivery and dose-response alignment. The literature on nudge theory demonstrates that effect sizes are moderated by cognitive load, health literacy, and structural determinants such as access to pharmacy services.
Moreover, the heterogeneity of patient archetypes-particularly those with multimorbidity and low socioeconomic status-demands stratified intervention design. A one-size-fits-all SMS protocol is statistically insufficient to address the polypharmacy burden, which exhibits a non-linear decay curve in adherence.
Future iterations must integrate ecological momentary assessment (EMA) via wearable biosensors to dynamically adapt behavioral triggers in real time, thereby achieving micro-personalization at scale.
Write a comment