DVT Risk Calculator
How Obesity Affects Your DVT Risk
Enter your BMI to see your risk level based on the latest medical research. Remember: even 5-10% weight loss can significantly reduce your risk.
Your DVT Risk Assessment
Your current DVT risk is times higher than normal-weight individuals (BMI 18.5-24.9).
Based on medical studies, a 5-10% weight loss could reduce your risk by up to %.
Recommended Actions
Quick Takeaways
- Obesity roughly doubles the odds of developing deep vein thrombosis (DVT) compared with normal‑weight individuals.
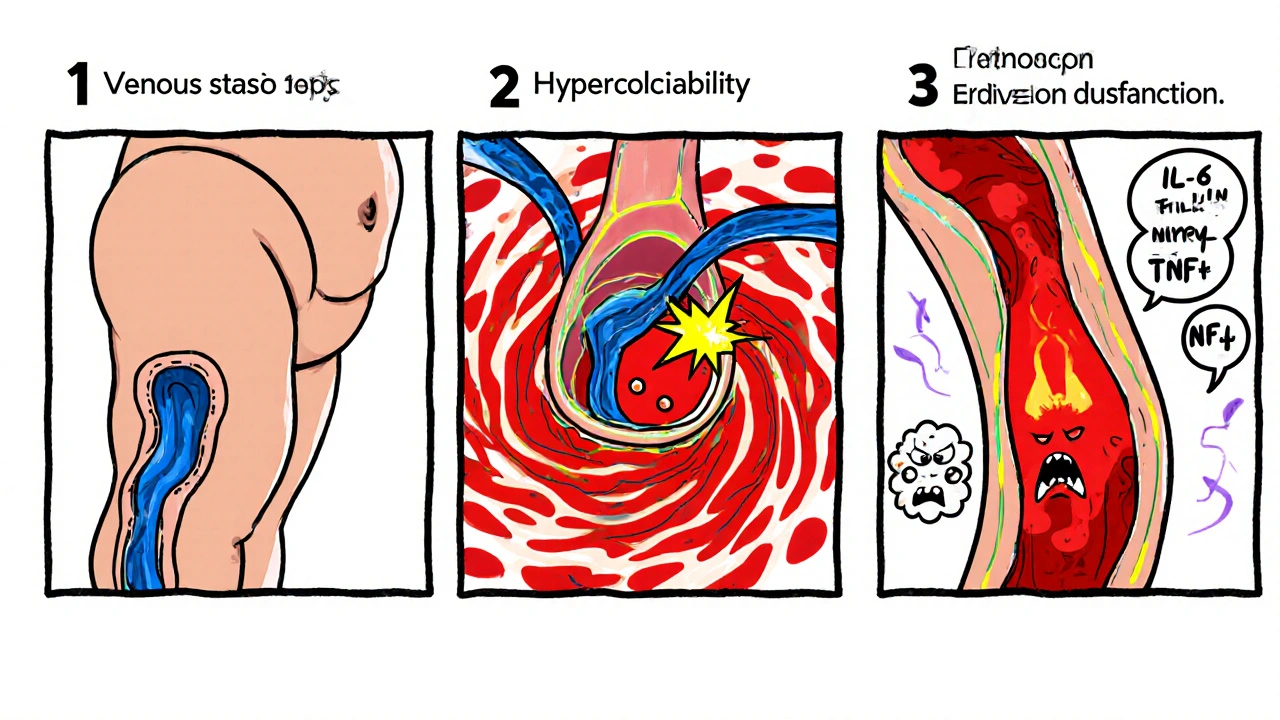
- Three main physiological pathways link excess weight to clot formation: venous stasis, hypercoagulability, and endothelial dysfunction.
- Even modest weight loss (5‑10% of body weight) can lower DVT risk noticeably.
- Compression stockings, regular movement, and proper hydration are simple daily actions that help protect the veins.
- Seek medical advice promptly if you notice unexplained swelling, pain, or discoloration in a leg.
What is Obesity?
Obesity is a chronic medical condition characterized by excess body fat, typically defined by a body mass index (BMI) of 30 kg/m² or higher. It results from an energy imbalance-consuming more calories than the body expends-combined with genetic, hormonal, and environmental factors. In 2024, over 42% of U.S. adults fell into the obese category, making it a leading driver of cardiovascular disease, type 2 diabetes, and, importantly for this article, venous thromboembolism.
Understanding Deep Vein Thrombosis
Deep vein thrombosis (DVT) is a clot that forms in a deep vein, most commonly in the legs. If the clot dislodges, it can travel to the lungs and cause a pulmonary embolism-an emergency with a mortality rate of up to 15% in untreated cases. DVT accounts for roughly 100,000 hospitalizations annually in the United States.
How Excess Body Weight Fuels DVT
The link between obesity and DVT isn’t just correlation; it’s rooted in three inter‑related physiological changes.
- Venous Stasis - Extra tissue mass compresses veins, especially in the pelvis and thighs, slowing blood flow. This stagnation is a classic element of Virchow's triad. Venous Stasis grows as abdominal girth expands, making clot formation more likely.
- Hypercoagulability - Obese individuals often have higher levels of fibrinogen, factor VII, and P‑selectin, all of which tip the blood toward clotting. This state is called Hypercoagulability and is measurable through elevated D‑dimer and thrombin‑antithrombin complexes.
- Endothelial Dysfunction - Fat tissue releases inflammatory cytokines (IL‑6, TNF‑α) that damage the inner lining of veins. The compromised Endothelial Dysfunction reduces nitric oxide production, impairing the vessel’s natural anti‑clot mechanisms.
Beyond these three pillars, obesity often co‑exists with Metabolic Syndrome, a cluster of hypertension, dyslipidemia, and insulin resistance that further amplifies clot risk. Together, they create a perfect storm for venous thromboembolism (VTE).
Numbers that Matter - Risk Statistics
Large cohort studies have quantified the added danger. Below is a snapshot of incidence rates drawn from the 2023 National Health and Nutrition Examination Survey (NHANES) analysis.
| BMI Category | Incidence Rate | Relative Risk vs. Normal‑Weight |
|---|---|---|
| Normal weight (18.5-24.9 kg/m²) | 2.3 | 1.0 (reference) |
| Overweight (25.0-29.9 kg/m²) | 4.1 | 1.8 |
| Obesity (30.0-34.9 kg/m²) | 6.9 | 3.0 |
| Severe Obesity (≥35 kg/m²) | 10.2 | 4.4 |
Interpretation: an individual with a BMI of 35 kg/m² faces more than four times the risk of a clot compared with someone of normal weight. That’s a stark reminder why weight management matters for vein health.
Spotting the Warning Signs
Early detection saves lives. Common DVT symptoms include:
- Swelling in one leg that feels tight or heavy.
- Pain that worsens when the leg is extended or when you stand for long periods.
- Red or bluish discoloration of the skin over the affected area.
- Warmth to the touch along the vein.
Because obesity can mask these signs-fat tissue may hide swelling-regular self‑checks become essential, especially after prolonged travel or after surgery.
Reducing the Risk - What Can You Do?
Risk reduction is a layered approach, targeting the three mechanisms we discussed.
- Weight Loss - Clinical trials show that a 5‑10% reduction in body weight lowers fibrinogen levels and improves venous flow. Even modest calorie deficits (500 kcal/day) can achieve this over 3-6 months.
- Movement and Hydration - Stand up and walk for a few minutes every hour, especially during long flights or desk work. Staying hydrated keeps blood less viscous, counteracting hypercoagulability.
- Compression Stockings - Graduated Compression Stockings (15‑30 mmHg) apply gentle pressure, encouraging blood to move upward toward the heart. They’re especially useful post‑surgery.
- Medical Prophylaxis - For high‑risk patients (e.g., recent orthopedic surgery, active cancer), doctors may prescribe Anticoagulation Therapy such as low‑molecular‑weight heparin or direct oral anticoagulants for a limited period.
- Lifestyle Changes - Incorporate at‑least‑150 minutes of moderate‑intensity aerobic activity per week. Pair this with strength training to improve muscle pump action in the legs.
Putting these steps into a routine can turn a high‑risk profile into a manageable one.
When to See a Doctor
If you notice any of the leg symptoms listed above, especially if they persist for more than 24 hours, schedule a medical evaluation promptly. Diagnostic tools include duplex ultrasound-an imaging test that can spot clots as small as 2 mm. Your clinician may also order a D‑dimer blood test to rule out clotting activity.
Patients with a known history of DVT should discuss long‑term prevention strategies with their physician, as recurrent episodes are more common in the obese population.
Key Takeaways Recap
- Obesity significantly raises DVT risk through venous stasis, hypercoagulability, and endothelial dysfunction.
- Risk climbs from 1× in normal‑weight individuals to over 4× in severe obesity.
- Weight loss, regular movement, compression therapy, and, when needed, anticoagulants are proven countermeasures.
- Early symptom recognition and timely medical care are vital to prevent dangerous pulmonary embolism.
Does losing just a few pounds really lower my DVT risk?
Yes. Research shows that a 5‑10% reduction in body weight can cut fibrinogen levels by up to 12% and improve venous return, translating to a measurable decrease in clot‑forming potential.
Are compression stockings necessary for everyone who is overweight?
They are most beneficial after prolonged immobility (e.g., long flights, post‑surgery) or if you have a history of DVT. For everyday use, a well‑fitted pair can still improve leg circulation.
Can obesity cause DVT even without other risk factors?
Absolutely. The three mechanisms-stasis, hypercoagulability, and endothelial damage-can each arise solely from excess adipose tissue, making obesity an independent risk factor.
Is there a specific BMI threshold where DVT risk spikes?
Risk begins to rise noticeably at a BMI of 30 kg/m² (the obesity cut‑off) and climbs sharply above 35 kg/m², where the relative risk can exceed four times that of normal‑weight individuals.
What role does exercise play in preventing DVT for obese adults?
Exercise activates the calf muscle pump, pushing blood out of the deep veins. Even low‑impact activities like walking or swimming can offset the stagnation caused by excess weight.



Comments
Rakhi Kasana
October 19, 2025
Listen, the data isn’t just numbers on a page; it’s a warning bell for anyone carrying extra weight. Every extra pound adds pressure on the veins, turning a simple walk into a silent threat. The triple‑hit of stasis, hypercoagulability, and endothelial damage isn’t a myth – it’s science. If you’re ignoring the risk, you’re basically flirting with a clot that could pop up at any moment. So take the guide seriously and start making those small moves now.
Sarah Unrath
October 19, 2025
i think you r right but many ppl dont see the link between weight and clot risk it’s real
James Dean
October 19, 2025
From a broad view health is a balance and obesity tips that balance toward clot formation the body’s own machinery becomes overactive yet we often ignore the quiet signals that tell us something is off in the veins
Bobby Marie
October 20, 2025
Exactly, the calf muscle pump matters more than most think. Simple steps can keep blood flowing.
Christian Georg
October 20, 2025
Here’s a quick checklist you can actually use: stay hydrated, move at least every hour, wear graduated compression if you’re on a long flight, and aim for a modest 5‑10% weight loss. Even a small calorie deficit can shrink those inflammatory markers over a few months 😊. Remember, consistency beats intensity when you’re trying to keep the blood thin.
Leo Chan
October 20, 2025
Great points! I’ve seen friends cut their risk just by strolling during work breaks and keeping a water bottle handy. It’s amazing how those tiny habits add up to big protection for the veins. Keep sharing the tips – the more we know, the healthier we all become!
jagdish soni
October 20, 2025
One must contemplate the metaphysical implications of a clot - a silent rebellion of the circulatory system against the tyranny of excess adipose tissue. When the body yields to the hedonistic comfort of caloric surplus, it spawns a cascade of coagulative whispers that eventually crescendo into danger.
Latasha Becker
October 20, 2025
To elucidate, the hypercoagulable state in obesity is mediated by elevated levels of fibrinogen, factor VIIa, and plasminogen activator inhibitor‑1, which collectively augment thrombin generation and impair fibrinolysis. Moreover, adipose‑derived cytokines such as IL‑6 potentiate hepatic synthesis of acute‑phase reactants, further skewing the hemostatic equilibrium toward thrombogenesis.
parth gajjar
October 20, 2025
It is as if the very essence of the flesh conspires against the veins, a tragic ballet where fat drapes the vessels in a suffocating embrace, stalling the river of life within. The heart’s lament echoes in every stagnant pool of blood, a dirge for the lost mobility of the body.
Maridel Frey
October 20, 2025
In clinical practice, I advise patients to incorporate graduated compression stockings with a pressure gradient of 15‑30 mmHg, particularly after orthopedic procedures. Coupled with a structured walking program of at least 150 minutes per week, this regimen demonstrably reduces venous stasis and improves endothelial function. Regular monitoring of D‑dimer levels can also aid in early detection of hypercoagulability.
Madhav Dasari
October 20, 2025
Dude, I totally get the struggle – sitting all day feels like a trap, but those quick leg lifts or marching in place can be a game‑changer. Trust me, the surge of blood back to the heart feels like a tiny victory each time. Keep at it and you’ll see the swelling melt away.
DHARMENDER BHATHAVAR
October 20, 2025
Maintain hydration, schedule hourly ambulation, and consider compression therapy for high‑risk individuals.
Kevin Sheehan
October 20, 2025
While some dismiss weight as merely cosmetic, the physiological cascade it triggers is a ruthless assault on vascular integrity, and we cannot afford complacency in the face of such evidence.
Jameson The Owl
October 20, 2025
The mainstream narrative that downplays the clotting hazards associated with excess adiposity is nothing short of a calculated misinformation campaign designed to preserve the status quo of a food‑industrial complex that thrives on overconsumption.
The scientific literature repeatedly demonstrates that individuals with a BMI exceeding thirty not only exhibit elevated fibrinogen and factor VII levels but also suffer from chronic endothelial dysfunction that predisposes them to venous thromboembolism.
Yet policy makers continue to allocate resources toward superficial wellness initiatives rather than enforcing mandatory screening protocols for hypercoagulability in obese populations.
The failure to recognize venous stasis as a direct consequence of abdominal girth expansion reflects a broader ignorance of Virchow's triad among healthcare administrators.
In addition, the pervasive use of sedentary transport and prolonged air travel amplifies the risk, creating a perfect storm that is ignored by airlines that profit from the very passengers at risk.
Compression stockings, a low‑cost intervention, are seldom recommended unless patients have a documented history of deep vein thrombosis, despite evidence that prophylactic use can halve the incidence of clots in high‑risk cohorts.
Moreover, the entrenched belief that modest weight loss is inconsequential is debunked by randomized trials showing a ten percent reduction in body mass leads to a measurable decline in D‑dimer concentrations.
The genetic predisposition to thrombosis does not absolve individuals from lifestyle accountability; rather it underscores the necessity for targeted education and personalized risk assessments.
Healthcare systems worldwide should integrate mandatory education on the triad of stasis, hypercoagulability, and endothelial injury into primary care curricula to arm clinicians with actionable knowledge.
Failure to do so not only endangers millions but also imposes an avoidable economic burden on insurers who foot the bills for preventable hospitalizations.
The confluence of obesity, metabolic syndrome, and sedentary behavior creates a synergistic effect that exponentially raises the odds of clot formation beyond the additive sum of each factor.
Patients often misinterpret the subtle swelling of a leg as inconsequential, unaware that the underlying thrombus may be propagating silently toward the pulmonary circulation.
Early ultrasound screening, when paired with an elevated D‑dimer, can identify occult thromboses before catastrophic embolic events occur.
Public health campaigns must therefore shift from generic diet advice to precise, evidence‑based strategies that include movement prompts every hour and hydration reminders.
Only through coordinated effort among clinicians, policymakers, and individuals can we dismantle the hidden threat of obesity‑induced deep vein thrombosis and safeguard vascular health for future generations.
Monika Bozkurt
October 20, 2025
In summary, integrating a multidisciplinary approach that combines caloric moderation, structured aerobic activity, and evidence‑based compression therapy constitutes the optimal strategy to mitigate obesity‑related venous thromboembolism risk.
Write a comment