Sticking with your meds isn’t just about remembering to take them
It’s about living with them. If you’ve been on chronic medication for months or years-whether for high blood pressure, diabetes, rheumatoid arthritis, or something else-you know it’s not just a daily habit. It’s a constant mental load. The pills, the side effects, the fear of forgetting, the cost, the feeling that your body is now tied to a schedule. And when you miss a dose, it’s not just a slip. It feels like failure.
The truth? You’re not lazy. You’re not broken. You’re human. And the people who stick with their meds long-term aren’t superheroes. They’ve learned how to cope.
Problem-solving: The most powerful tool you already have
Research shows that problem-solving, or active coping, is the single most effective strategy for sticking with your meds. In studies, 78% of people who used this approach showed better adherence. What does that look like in real life?
It’s not about willpower. It’s about removing friction.
- You notice you keep forgetting your afternoon pill. So you start keeping it in your toothbrush holder. Now, every time you brush your teeth, you take it.
- You’re overwhelmed by five different pills at breakfast. You ask your pharmacist if any can be combined. Turns out, yes-two of them come in one tablet now.
- You can’t afford your medication. You don’t just stop. You call your doctor’s office and ask about RxAssist.org or patient assistance programs. You don’t beg. You problem-solve.
This isn’t theoretical. A study of rheumatoid arthritis patients found those who scored higher on active coping had significantly better adherence. Their scores weren’t just higher-they were statistically significant. And it wasn’t because they were more disciplined. It was because they changed their environment to match their needs.
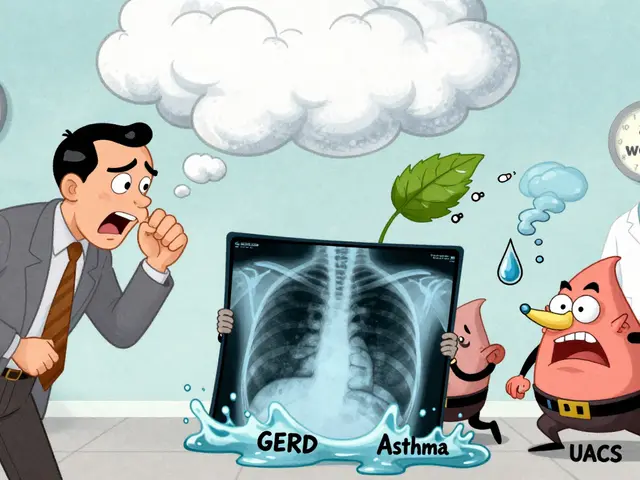
Emotion-focused coping: It’s okay to feel tired of this
Chronic illness doesn’t come with a warning label. One day you’re fine. The next, you’re managing a condition that never sleeps. It’s exhausting. And that exhaustion often turns into resentment.
Emotion-focused coping isn’t about ignoring how you feel. It’s about acknowledging it and giving yourself space to process it.
- You cry after taking your pills one morning. Instead of beating yourself up, you write it down: “Today, I hate that I need these.” Then you put the journal away. No guilt.
- You listen to music that makes you feel strong while you sort your pill organizer. You turn a chore into a ritual.
- You tell your partner, “I’m feeling really overwhelmed with this right now.” And you don’t apologize for it.
Studies show 69% of people who used emotion-focused coping had better adherence. Why? Because suppressing emotions drains energy. Naming them frees it up.
Support seeking: You don’t have to do this alone
Many people think asking for help means admitting weakness. It doesn’t. It means you’re smart enough to know you can’t do everything alone.
Team-based care-where pharmacists, doctors, nurses, and social workers work together-has been shown to boost adherence from 74% to 89% after just 12 months. That’s not magic. That’s structure.
Here’s what works:
- Ask your pharmacist to call you when your refill is due. Most pharmacies offer this for free.
- Join a support group-even online. Talking to someone who knows what it’s like to forget pills at 3 a.m. is better than any pamphlet.
- Bring a friend to your next appointment. They can remember questions you forgot to ask.
One study found women were over four times more likely to stick with their meds than men. Why? Not because they were more compliant. Because they were more likely to reach out for help.
Understanding your meds: Knowledge is armor
When you don’t understand why you’re taking something, it’s easy to stop. “Is this even working?” “Why do I need this if I feel fine?”
Seeking understanding isn’t about reading medical journals. It’s about asking simple questions:
- “What does this pill actually do in my body?”
- “What happens if I skip it for a week?”
- “Are there cheaper versions?”
Doctors don’t always explain this well. But if you ask, they’ll answer. And when you know the reason behind the pill, it stops feeling like an intrusion. It becomes part of your story.
Problem avoidance: The trap most people fall into
This is the silent killer of adherence. It’s when you tell yourself:
- “I’ll start again tomorrow.”
- “I don’t feel sick, so maybe I don’t need it.”
- “It’s too expensive-I’ll just skip a few doses.”
Half the studies on problem avoidance show it leads to worse adherence. And the other half? They show mixed results. That’s because sometimes, avoiding the problem works-for a little while. But chronic conditions don’t wait. They don’t care if you’re having a bad day. They keep ticking.
Problem avoidance isn’t failure. It’s a signal. It’s your brain screaming, “This is too hard.” And the right response isn’t to shame yourself. It’s to ask: “What’s making this so hard? And how can I fix it?”
What actually helps in the real world?
Let’s cut through the noise. Here’s what works, based on real data-not theory:
- Simplify your regimen. Ask your doctor if you can switch to once-daily pills or combination tablets. Reducing the number of pills you take daily is one of the biggest predictors of adherence.
- Use a pill organizer. Not just any one-get one with alarms or a lock. Some even send texts to your phone.
- Know your cost options. Generic drugs work just as well. Ask for them. Use RxAssist.org or your pharmacy’s discount program. You’re not being cheap-you’re being smart.
- Set phone reminders. Set two: one for when to take it, one as a backup 30 minutes later.
- Track your mood. Keep a simple log: “Took meds today? Yes/No. How did I feel?” After a month, patterns emerge.

Why some people still struggle-even with all the tools
Here’s the hard part: coping strategies aren’t magic bullets. A study of rheumatoid arthritis patients found that even when people used active coping, the effect disappeared when adjusted for age, income, and disease length. That means:
- If you’re older, you might need more support.
- If you’re on a tight budget, no amount of reminders will help if the pills cost $500 a month.
- If you’ve had this condition for 10 years, the fatigue is real-and it’s not just mental.
That’s why the best solutions combine coping strategies with real-world fixes: lower prices, simpler dosing, better access to care. No one should have to choose between eating and taking their meds.
What to do next
Don’t try to fix everything at once. Pick one thing.
- If you forget pills often: get a pill organizer with a timer.
- If you feel overwhelmed: talk to your pharmacist about simplifying your regimen.
- If you’re scared to ask for help: write down one question and bring it to your next appointment.
Adherence isn’t about being perfect. It’s about being consistent. And consistency doesn’t come from discipline. It comes from systems, support, and self-compassion.
You’re not alone in this
Millions of people are managing chronic meds right now. Some days are good. Some days are rough. That’s normal. The goal isn’t 100% adherence every single day. It’s staying in the game. One pill at a time.
Why do I keep forgetting to take my medication even though I know it’s important?
Forgetting isn’t about being careless-it’s about how your brain handles routine. When something becomes automatic, your brain stops paying attention. The fix isn’t to try harder. It’s to make the action harder to ignore. Use a pill organizer with an alarm, link your pill to a daily habit like brushing your teeth, or set two phone reminders 30 minutes apart. These aren’t tricks-they’re science-backed tools.
Can I stop taking my meds if I feel fine?
No-not without talking to your doctor. Many chronic medications work silently. Blood pressure pills don’t make you feel better-they prevent damage. Diabetes meds don’t cure the disease-they keep your blood sugar from spiking. Stopping them can lead to long-term complications like kidney damage, heart attacks, or strokes. Feeling fine is actually a sign the meds are working.
My pills are too expensive. What can I do?
You’re not alone. Many people struggle with this. Ask your pharmacist if a generic version is available. Check RxAssist.org for patient assistance programs. Some drug companies offer free or discounted meds if you meet income guidelines. You can also ask your doctor about step-therapy-starting with a cheaper, equally effective drug. Never stop taking your meds because of cost. Talk to someone. There are options.
Is it normal to feel resentful about taking meds every day?
Yes. It’s completely normal. Chronic illness changes your identity. You’re no longer just “you”-you’re “the person who takes pills.” That can feel like a loss. Journaling, talking to others in support groups, or even just saying out loud, “I hate this,” can help. You don’t need to be grateful. You just need to be honest. And you’re allowed to feel this way.
Do coping strategies really make a difference?
Yes-especially problem-solving and emotion-focused coping. Studies show 78% of people who actively solve barriers to taking their meds improve adherence. Those who use emotional strategies like talking about their feelings or creating rituals also see big gains. The key isn’t just doing these things once. It’s making them part of your daily rhythm. Like brushing your teeth, but for your health.




Comments
Kane Ren
November 23, 2025
This hit different. I’ve been on blood pressure meds for 5 years and I used to feel like a failure every time I missed one. Then I started keeping my pillbox next to my coffee maker. Now I take it while I wait for my brew. Small changes, big difference. You’re not broken-you’re just human.
Charmaine Barcelon
November 23, 2025
You people are so lazy!! Why don’t you just SET A REMINDER?!?!?!?!?!!? It’s not rocket science!!
Karla Morales
November 24, 2025
I appreciate the data-driven approach, but I’m concerned about the lack of longitudinal follow-up in the cited studies. The 78% adherence rate is impressive, but was it sustained beyond 6 months? Also, did they control for socioeconomic status? Because let’s be real-$500/month isn’t just a ‘cost issue,’ it’s a systemic failure. 📊💔
Javier Rain
November 25, 2025
YES. This. I used to skip my RA meds because I ‘felt fine.’ Then I started writing one sentence in my phone notes every time I took them: ‘Today, I chose my future.’ It sounds cheesy, but it stuck. You don’t need willpower-you need a reason that feels like yours. And you’re allowed to hate the system. Just don’t let it win.
Laurie Sala
November 27, 2025
I just cried reading this. I’ve been taking these pills for 12 years and I’ve never told anyone how much I hate them. I feel like my body is a prison. I’m so tired of being the person who needs help. I just… I just wish I could be normal again. 😭
Lisa Detanna
November 28, 2025
As someone from a culture where asking for help is seen as weakness, this changed everything for me. I used to think I had to suffer quietly. But when I finally told my sister I needed help sorting my pills? She showed up with a labeled organizer and a playlist of old Bollywood songs. We danced while I took my meds. I didn’t know that was allowed. Thank you.
Demi-Louise Brown
November 29, 2025
Simplification is key. One pill. One time. One routine. That’s the formula. No need for complexity. Align the habit with an existing behavior. Brush teeth? Take pill. Eat breakfast? Take pill. Consistency > perfection. Track progress weekly. Not daily. Less pressure. More sustainability.
Suresh Ramaiyan
November 30, 2025
I’ve been on antihypertensives since I was 32. I’m 58 now. What helped me most wasn’t the alarms or the organizers. It was realizing I wasn’t taking pills to live longer-I was taking them to live better. To play with my grandkids without getting winded. To walk without pain. The pills aren’t the enemy. The silence around them is. We need to talk more. Not just about adherence. About dignity.
Katy Bell
December 1, 2025
I used to feel so guilty for missing doses… until I realized I wasn’t failing my meds-I was failing the idea that I had to be perfect. Now I just say, ‘Okay, I missed today. What’s one thing I can do tomorrow to make it easier?’ And I move on. No shame. No drama. Just… next.
Ragini Sharma
December 2, 2025
i rlly dont get why ppl make this so hard?? just put ur pills in ur phone case n set a remindr!! its not that hard?? why u all so dramatic?? 😅
Henrik Stacke
December 3, 2025
I must respectfully suggest that while the psychological frameworks presented are valuable, they operate within a context of structural inequity. In the UK, I’ve seen patients on insulin rationing doses due to prescription charges. No amount of problem-solving can substitute for universal healthcare access. The burden should not fall solely on the individual. Systemic reform is not optional-it is ethical.
Olanrewaju Jeph
December 4, 2025
This is exactly what my grandmother taught me: 'Medicine is not punishment. It is protection.' She took her pills every day for 40 years. Never missed one. Not because she was strong-but because she knew her body was still hers, even when it needed help. That’s the real secret: You’re not losing yourself. You’re protecting who you are.
Write a comment