Prior Authorization Risk Calculator
This tool estimates your risk of dangerous treatment delays based on your insurance plan and medical condition. Prior authorization delays can be life-threatening for time-sensitive conditions.
Imagine you’re prescribed a life-saving medication. Your doctor says it’s the right choice. But you can’t fill the prescription for weeks - not because you can’t afford it, but because your insurance company needs more paperwork. This isn’t rare. It’s happening to millions right now. And in some cases, those delays are killing people.
What Prior Authorization Really Does
Prior authorization is supposed to be a safety net: a check to make sure you’re getting the right treatment at the right cost. In theory, it stops unnecessary MRIs, expensive drugs, or risky surgeries. But in practice, it’s become a bottleneck. Health insurers - especially Medicare Advantage and private plans - require doctors to jump through hoops before they can treat you. For specialty drugs costing over $1,000 a month, you might have to try two cheaper alternatives first. Even if those didn’t work for you last year. Even if your doctor says they won’t work now.It’s not just medications. MRIs, physical therapy, oxygen tanks, even certain lab tests often need approval. And the system isn’t built for speed. As of 2024, nearly 85% of prior authorization requests still go out by fax. Yes, fax. Doctors’ offices spend an average of 16 hours a week just chasing approvals. That’s not time spent with patients. That’s time spent on hold, filling out forms, or resubmitting the same request because the insurer lost the first copy.
Why Delays Are Deadly
The real danger isn’t the paperwork. It’s the time lost while waiting.For someone with cancer, a delay of more than 28 days in starting treatment increases the risk of death by 17%. For transplant patients on immunosuppressants, even a week without their medication can trigger organ rejection. Diabetic patients waiting for insulin pumps have ended up in emergency rooms with diabetic ketoacidosis - all because their insurance took 11 days to approve the device. These aren’t hypotheticals. They’re documented cases, tracked by hospitals and reported by nurses on forums like Reddit.
It’s not just life-threatening conditions. People with chronic pain, autoimmune diseases, or mental health disorders are also caught in the gap. If your anti-rejection drug or antidepressant gets denied, you don’t just feel worse - your body starts to break down. Some patients give up. They stop taking the medication. They stop calling the insurance company. They just wait - until something worse happens.
Who’s Affected the Most
This isn’t equal across the board. Medicare Advantage plans require prior authorization for nearly 80% of specialty drugs. Medicaid varies wildly - one state might approve a drug in two days, another might take three weeks. Commercial insurers are faster on average, but still take over four business days for a decision. And for low-income patients, the delay isn’t just medical - it’s financial. If you’re working hourly jobs, missing a day to call insurance means missing pay. If you’re caring for a child or elderly parent, you can’t afford to sit on hold for hours.Studies show 82% of patients abandon treatment because of prior authorization hurdles. That’s not laziness. That’s exhaustion. That’s the system working exactly as designed - to discourage expensive care, even if it means sacrificing health.

How Providers Are Fighting Back
Doctors aren’t sitting still. Many clinics now have dedicated prior authorization teams. Instead of one nurse handling all the paperwork, they assign specialists who know exactly what each insurer wants. They use standardized templates - pre-filled forms that cut documentation time by 40%. They check benefits before the patient even leaves the exam room. That alone reduces the number of requests by nearly a third.Some practices keep a small stock of short-term medication samples - a 7- to 14-day supply - to bridge the gap while approval is pending. It’s not perfect. It costs money. But it’s saved lives. One oncology clinic in Ohio started this practice after a patient died waiting for a drug. Now, every new cancer patient gets a starter pack on day one. The insurance approval comes later. The treatment doesn’t.
Electronic systems are making a difference. Practices using digital prior authorization see approval times drop from over five days to under two. But only 15% of all requests are processed electronically. The rest? Still faxed. Still mailed. Still lost.
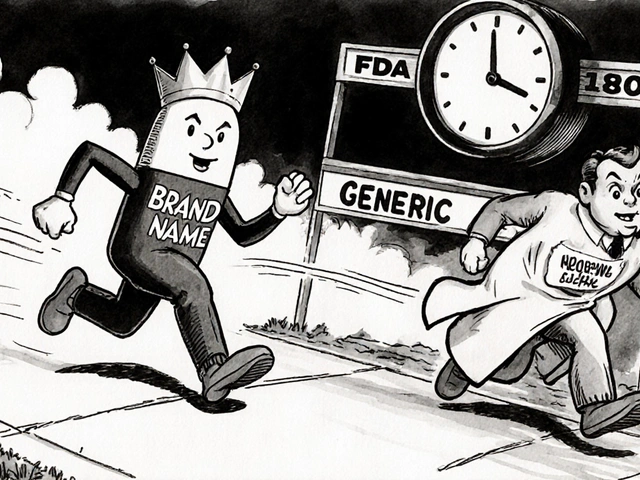
What’s Changing - and What’s Not
There’s hope. In January 2024, the Centers for Medicare & Medicaid Services (CMS) announced a new rule: by December 2026, all Medicare Advantage and Medicaid managed care plans must use electronic systems with real-time approval capabilities. That’s a big deal. It means a doctor could request approval during a patient visit and get an answer before they leave the office.States are moving too. California now requires emergency authorizations to be approved within 24 hours. Other states are limiting prior authorization to only the most expensive or risky treatments. The AMA is pushing federal legislation to ban prior authorization for patients who are already stable on a medication - no more forcing someone to switch drugs just because a new, slightly cheaper one exists.
But progress is slow. As of mid-2024, 63% of Medicaid programs still rely on fax machines. Only 41% of physicians say the process has improved. And until every insurer is on the same system, the gaps will remain.

What Patients Can Do
You don’t have to wait passively. Ask your doctor at the time of prescription: "Will this need prior authorization?" That simple question cuts delays by 63%. If it does, ask for a copy of the clinical justification letter. Keep it. If the insurer denies it, you’ll need it to appeal.Call your insurer. Don’t wait for them to call you. Ask for the name of the person handling your case. Get a reference number. Write down every call - date, time, who you spoke to, what they said. If you’re denied, file an appeal immediately. Most insurers have a 180-day window, but the sooner you act, the better.
Look into patient assistance programs. Many drug manufacturers offer free or low-cost medication during authorization delays. Nonprofits like the Patient Access Network Foundation or the HealthWell Foundation can help cover costs. You don’t have to pay out of pocket while waiting.
If you’re on Medicare Advantage, know your rights. You have the right to an expedited review if your condition is urgent. You can ask for it in writing. And if you’re still stuck, contact your state’s insurance commissioner’s office. They can intervene.
The Bigger Picture
This isn’t just about paperwork. It’s about trust. Patients trust their doctors. They trust the system to help them get better. But when the system makes them wait - when it forces them to risk their health to save money - that trust breaks.The cost of prior authorization isn’t just $31 billion in administrative waste. It’s in lost workdays, emergency room visits, hospitalizations, and deaths that could have been avoided. Employers lose $12.4 billion a year in productivity because workers are too sick to show up. The system isn’t broken - it was built this way. To control costs. But it’s controlling lives, too.
Change is coming. Electronic systems. Faster rules. Better tools. But until every single request is processed in real time, the danger remains. The next person waiting for a prescription might be your neighbor. Your parent. Your friend. Don’t assume someone else is handling it. Ask. Advocate. Push. Because when it comes to your health, waiting isn’t an option.
What is prior authorization and why does it delay treatment?
Prior authorization is when your insurance company requires approval before covering certain medications or procedures. It’s meant to prevent unnecessary care, but in practice, it creates delays because providers must submit paperwork - often via fax - and wait days or weeks for a decision. These delays can be dangerous for time-sensitive conditions like cancer, epilepsy, or autoimmune disorders, where even a few days without treatment can lead to serious health events.
Which health plans require prior authorization the most?
Medicare Advantage plans require prior authorization for about 83% of specialty drugs. Commercial insurers use it for 60% of specialty medications and 20-30% of brand-name drugs. Medicaid varies widely by state - some require it for less than 15% of prescriptions, others for over 85%. Medicare Parts A and B generally do not require prior authorization, which is why many patients switch to Medicare Advantage for extra benefits - unaware of the trade-off in access speed.
How long do prior authorization delays usually take?
For non-urgent requests, the average approval time is 4.7 to 7.2 business days, depending on the insurer. Medicaid takes the longest, averaging over 7 days. Medicare Advantage is around 5 days. Urgent cases should be approved within 72 hours - but studies show nearly 40% of urgent requests still take longer than that. In reality, many patients wait over a week, especially if the first request is denied and an appeal is needed.
Can prior authorization cause patients to stop taking their medication?
Yes. According to physician surveys, 82% of patients abandon treatment because of prior authorization delays. Some can’t afford to pay out of pocket during the wait. Others get overwhelmed by phone calls and paperwork. One study found patients make an average of 3.7 calls per authorization attempt. When the system feels impossible to navigate, many simply give up - even if it means worsening their condition.
What can I do if my prior authorization is denied?
File an appeal immediately. Request the reason for denial in writing. Ask your doctor to write a letter of medical necessity. If you’re on Medicare Advantage or Medicaid, you have the right to an expedited review if your condition is urgent. You can also contact your state’s insurance commissioner’s office - they can pressure the insurer to act. Meanwhile, check if the drug manufacturer offers a patient assistance program to cover costs during the appeal.
Are electronic prior authorization systems better?
Yes. Practices using electronic systems see approval times drop from over five days to under two. They also reduce denial rates by 35% because the system flags missing information before submission. By 2026, federal rules will require all Medicare Advantage and Medicaid plans to use electronic systems with real-time decisions. Until then, ask your provider if they use one - and if not, push them to switch.
Is prior authorization ever helpful?
In rare cases, yes. It can prevent unnecessary surgeries or overprescribing of opioids. A small percentage of patients (about 12%) report that prior authorization helped them avoid costly, ineffective treatments. But these are exceptions. The overwhelming evidence shows that for most patients - especially those with chronic or life-threatening conditions - the risks of delay far outweigh the benefits of cost control.
What Comes Next
The future of prior authorization is moving toward automation - AI tools that predict what insurers will approve, systems that auto-fill forms, and real-time checks built into electronic health records. But technology alone won’t fix this. The real fix is policy: rules that limit prior authorization to only the most extreme cases, deadlines that are enforced, and penalties for insurers who ignore them.Until then, stay informed. Ask questions. Keep records. And if you’re a caregiver, advocate, or patient - don’t let silence be your answer. The system was designed to make you wait. Don’t let it win.



Comments
Isabelle Bujold
December 4, 2025
I’ve been working in oncology nursing for 18 years, and I’ve seen firsthand how prior auth delays kill. Not in dramatic ways-no headlines, no viral videos. Just quiet, slow deaths. A patient gets diagnosed, the doctor orders the drug, and then it’s a 14-day game of phone tag with the insurer. By day 10, they’re too weak to even sit up. By day 14, they’re in the ER with sepsis from neutropenia. And the worst part? The insurer approves it the next day. They approved it after the damage was done. We keep a folder of these cases. It’s not anecdotal. It’s systematic. And no, electronic systems won’t fix this until insurers stop designing the process to fail.
My clinic started giving out 7-day starter packs last year. We don’t wait. We don’t ask permission. We save lives first, paperwork later. The insurance company hates it. But they haven’t cut our contract yet. Maybe because we’ve documented every single case where we prevented a hospitalization. They’d rather pay for the drug than the ICU bed.
Patients need to know: if your doctor says it’s urgent, demand an expedited review. Write it down. Send it certified mail. And if they still drag their feet? Call your state’s insurance commissioner. They get hundreds of complaints a month. One more won’t hurt.
It’s not about being angry. It’s about being relentless. Because if you’re quiet, they assume you’re okay with it. And you’re not.
And yes-I’ve had patients cry because they couldn’t afford to pay out of pocket for a month of chemo. That’s not healthcare. That’s extortion dressed in a white coat.
Augusta Barlow
December 5, 2025
Let’s be real-this whole system is just Big Pharma and Big Insurance playing footsie while patients die. You think they don’t know this kills people? Of course they do. That’s the point. They don’t want you to get the good drugs. They want you to take the cheap generics that make them more money, even if they don’t work. And if you die? Well, that’s just a line item in their quarterly report. They’ve got algorithms that calculate how many deaths are ‘acceptable’ for profit margins. I’ve seen the internal memos. They’re not hiding it. They’re proud of it.
And don’t even get me started on the ‘electronic systems’ they’re rolling out. Those are just fancy fax machines with more buttons. The same people writing the forms are still in charge. They just made it look digital so they can charge hospitals more for ‘tech upgrades.’ It’s all theater. The real fix? Ban prior auth entirely for anything over $100 a month. Let doctors decide. Let patients live. Let the insurance companies go bankrupt trying to deny care. Maybe then they’ll learn.
Rebecca Braatz
December 6, 2025
If you’re reading this and you’re waiting on prior auth right now-you’re not alone. And you’re not broken. The system is broken. But here’s what you can do today: call your doctor’s office and ask for the prior auth team’s direct line. Most clinics have one now. Don’t call the insurer first. Call your provider. They know the game. They’ve done this a thousand times.
And if you’re a caregiver? Write down every call. Date. Time. Name. What they said. Even if it’s just ‘I’ll call you back.’ Keep it in a notebook. You’ll need it when you appeal. And you WILL appeal. Don’t let them wear you down.
There are free programs-Patient Access Network, HealthWell, even drug manufacturer coupons-that can cover your meds while you wait. Google them. Ask your pharmacist. They’re not secret. They’re just not advertised. Because if everyone knew, the insurers would lose money.
You are not a burden. You are not a hassle. You are a human being who deserves to live. And you have more power than you think. Start today. One call. One form. One appeal. You’ve got this.
Michael Feldstein
December 7, 2025
Just curious-how many of these prior auth delays are actually due to insurer bureaucracy vs. doctors not submitting complete info? I’ve seen cases where the doctor’s office sends a 3-page fax with half the fields blank, then wonders why it takes 10 days. Maybe part of the problem is on our end too?
I’m not defending insurers-hell, I’ve had my own family wait weeks for an MRI-but I wonder if some of the blame could be shared. Maybe better training for office staff? Or automated prompts in EHRs to flag missing docs before submission? Just thinking out loud.
jagdish kumar
December 9, 2025
The system is a mirror. It reflects our collective surrender to profit over humanity. We built this. We accepted it. We whispered, ‘Maybe it’s necessary.’ But no. It’s not. It’s evil dressed in spreadsheets.
michael booth
December 9, 2025
As a former claims analyst for a major insurer I can confirm the process is inefficient and outdated. Fax machines are still used because legacy systems are too expensive to replace. The real issue is interoperability. Every insurer uses different forms, different portals, different rules. Even if your doctor uses an electronic system, it might not talk to the insurer’s system. That’s why approvals take so long. It’s not malice-it’s technical debt. The CMS mandate for real-time systems by 2026 is the only thing that will fix this. We need standardized APIs. Not just digitization. Integration.
And yes, some doctors do submit incomplete forms. But that’s fixable with training and templates. The bigger problem? No one is held accountable for delays. There are no penalties. No KPIs for speed. Just cost savings. That’s the root.
Carolyn Ford
December 10, 2025
Oh please. Let’s not pretend this is about ‘patients dying.’ This is about lazy doctors who don’t want to do their job. If you’re prescribing a $12,000-a-month drug, maybe you should have considered cheaper alternatives FIRST. Prior auth exists to prevent overprescribing. You think insulin pumps are free? They’re not. And if you’re too busy to fill out a form, that’s your problem, not the insurer’s.
And don’t give me that ‘fax machines’ nonsense-my dentist uses e-signatures. Why can’t you? It’s not rocket science. It’s just that some providers are too lazy to adapt. Stop blaming the system. Start blaming the people who refuse to change.
Also, ‘patient assistance programs’? Those are taxpayer-funded handouts. Why should I pay for your expensive drugs? Maybe you should’ve saved for this. Just saying.
Heidi Thomas
December 11, 2025
My mom died waiting for prior auth. 17 days. She had stage 4 breast cancer. The drug worked. They approved it after she was gone. I’m not crying. I’m not asking for sympathy. I’m telling you: this kills. And if you’re still defending it, you’re part of the problem.
Write a comment