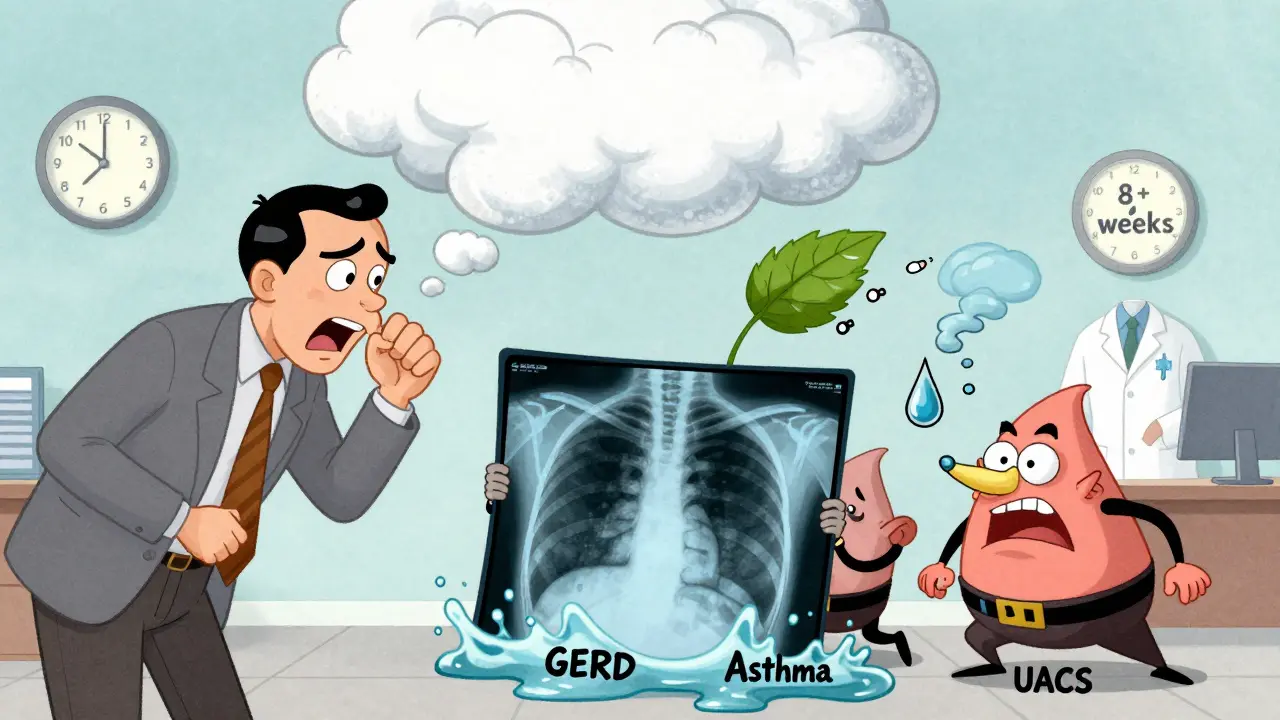
If you’ve been coughing for more than eight weeks, you’re not alone. About 1 in 10 adults deal with a persistent cough that won’t go away, no matter how many cough syrups they try. Most of the time, it’s not a cold, flu, or infection-it’s something deeper. And the real culprits? Three conditions you might not even connect to your cough: GERD, asthma, and postnasal drip (now called upper airway cough syndrome). Together, they cause 80% to 95% of chronic cough cases in people who don’t smoke or take certain blood pressure meds. The good news? Once you know what’s going on, relief can come in weeks-not months.
What Counts as a Chronic Cough?
A cough that lasts longer than eight weeks is officially chronic. That’s not just a rough estimate-it’s the standard set by the American College of Chest Physicians. Most people assume a long cough means they have bronchitis, allergies, or something lingering from a cold. But if you’ve been coughing for months and your chest X-ray came back normal, you’re likely dealing with one of the big three: GERD, asthma, or upper airway cough syndrome.
What makes this tricky is that the cough is often the only symptom. You might not have heartburn. You might not wheeze. You might not feel congested. That’s why so many people go from doctor to doctor, trying one treatment after another, without ever getting to the root cause.
Step 1: Rule Out the Red Flags
Before you start guessing whether it’s acid reflux or allergies, you need to make sure nothing serious is going on. The first step in any chronic cough workup is to look for warning signs that point to something more dangerous: coughing up blood, unexplained weight loss, night sweats, fever, or swelling in the legs. These could signal lung cancer, tuberculosis, or heart failure.
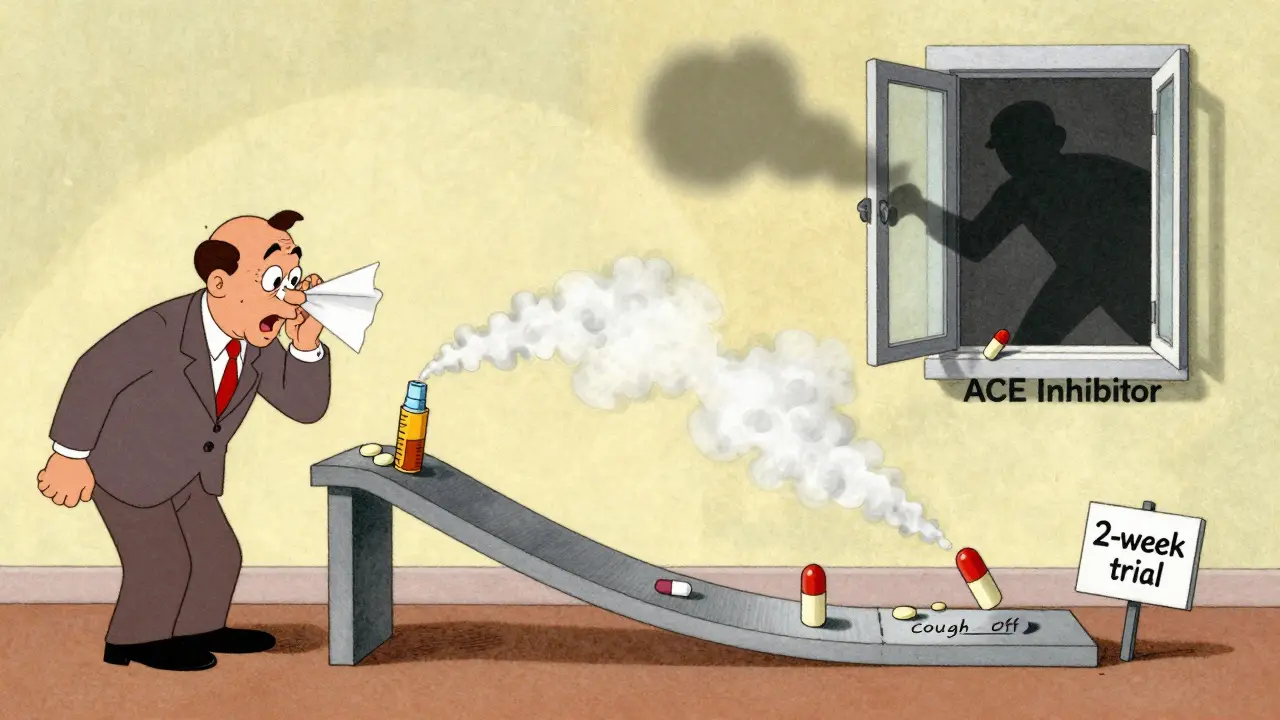
Another hidden trigger? Medications. About 5% to 35% of people who take ACE inhibitors-common blood pressure drugs like lisinopril or enalapril-develop a dry, hacking cough within days or months of starting them. If you’re on one of these and have a chronic cough, talk to your doctor about switching. It’s one of the easiest fixes.
Step 2: The Basic Tests
Once red flags are ruled out, the next step is simple: a chest X-ray and spirometry. You’d be surprised how much these two tests can tell you.
A chest X-ray won’t catch asthma or GERD, but it will rule out things like lung tumors, scarring, or infections that might be hiding in plain sight. If it’s normal-which it is in most cases-you’re already narrowing things down.
Spirometry measures how well your lungs move air in and out. It’s quick, non-invasive, and tells you if you have asthma. A person with asthma often has normal breathing most of the time, but their lungs react poorly to triggers. If the test shows obstruction, that’s a strong clue. If it’s normal, you might still have cough-variant asthma-where the only symptom is coughing. In that case, a methacholine challenge test might be needed. This test gently irritates the airways to see if they overreact. A positive result means asthma is likely.
Step 3: The Big Three-Diagnosing Each One
1. Asthma (Cough-Variant Asthma)
Asthma doesn’t always mean wheezing. In fact, about one in four adults with chronic cough have cough-variant asthma. This version of asthma doesn’t cause shortness of breath or chest tightness. It just makes your airways super sensitive, so even cold air, dust, or laughter triggers a coughing fit.
How do you know if it’s asthma? Start with a trial of inhaled corticosteroids-like fluticasone or budesonide-for 2 to 4 weeks. If your cough improves by at least half, asthma is likely the cause. If you’re still unsure, a positive methacholine challenge test (with a PC20 under 8 mg/mL) confirms it. About 60% to 80% of people with this type of asthma respond to treatment.
2. GERD (Silent Reflux)
GERD stands for gastroesophageal reflux disease. Most people think of heartburn when they hear that. But here’s the twist: up to 70% of people with GERD-related cough have no heartburn at all. This is called silent reflux. Stomach acid doesn’t always burn-it can trickle up and irritate the throat, triggering a cough reflex that’s been turned up too high.
Testing for GERD is messy. pH monitoring (a tiny tube in the esophagus) can show reflux, but it only catches abnormalities in half to 70% of cases. And even then, it doesn’t always prove the cough is caused by it.
So doctors use a different trick: a 4- to 8-week trial of high-dose proton pump inhibitors (PPIs), like omeprazole or esomeprazole, taken twice daily. If your cough improves, GERD is probably the culprit. But here’s the catch: about 35% to 40% of people improve on placebo pills. That’s why new guidelines from the American College of Gastroenterology (March 2024) now say: don’t start PPIs unless you have clear signs of reflux. If you’re not sure, try a questionnaire called the Hull Airway Reflux Questionnaire (HARQ). A score above 13 suggests laryngopharyngeal reflux with 80% accuracy.
3. Upper Airway Cough Syndrome (Postnasal Drip)
This used to be called postnasal drip syndrome. Now it’s called upper airway cough syndrome (UACS) because it’s not really about mucus dripping-it’s about nerves in the throat and nose being overly sensitive. Allergies, colds, pollution, or even dry air can trigger it.
The classic sign? A tickle in the back of the throat, frequent throat clearing, or feeling like something’s stuck there. It often gets worse at night or when lying down.
Diagnosis? Simple. Try a 2- to 3-week trial of a first-generation antihistamine (like chlorpheniramine) plus a decongestant (like pseudoephedrine). If your cough drops by 70% to 90%, you’ve got UACS. Second-generation antihistamines (like loratadine) don’t work as well-they don’t cross into the nervous system the same way. Nasal steroid sprays (like fluticasone) can also help, especially if allergies are involved.
Why the Order Matters
Doctors don’t test for all three at once. They follow a sequence because some treatments work faster and more reliably than others.
UACS responds quickest-usually within 1 to 2 weeks. Asthma takes 2 to 4 weeks. GERD takes the longest-up to 8 weeks. So the smart approach is to start with UACS, then asthma, then GERD. If the first one doesn’t help, move to the next. This avoids stacking medications, reduces side effects, and saves money.
But here’s the reality: 10% to 30% of people don’t improve with any of these three. That’s when things get harder. It could be chronic refractory cough (CRC), which means the nerves in the throat are just too sensitive. Or it could be something rare like vocal cord dysfunction, aspiration, or even a side effect of an old infection like pertussis (whooping cough).
What Doesn’t Work
Too many people get stuck in a loop of ineffective treatments. Antibiotics? Only 1% to 5% of chronic cough cases are caused by bacterial infections. You don’t need them. Over-the-counter cough suppressants? They rarely help. Honey? Might soothe your throat, but won’t fix the cause. Chest CT scans? They’re overused. A normal chest X-ray means a CT scan will almost never find cancer. The radiation exposure isn’t worth it.
And don’t ignore lifestyle. Smoking? Stop. Secondhand smoke? Avoid it. Dry indoor air? Use a humidifier. Eating late at night? Don’t. Spicy food? Cut back. These aren’t just tips-they’re part of the treatment.

What’s New in 2026
The field is changing fast. In December 2022, the FDA approved gefapixant, the first drug specifically for chronic refractory cough. It blocks a nerve signal that triggers coughing. In trials, it reduced coughing by 18% to 22%. Another drug, camlipixant, is under review and showed even better results-24.7% reduction in cough frequency.
Also, AI is stepping in. A 2023 study in Lancet Digital Health trained a computer to listen to coughs and tell whether they came from asthma or GERD. It got it right 87% of the time. Imagine a phone app that could help your doctor diagnose your cough just by recording it.
And terminology is shifting. “Postnasal drip” is being replaced with “upper airway cough syndrome” because it’s not about mucus-it’s about nerve sensitivity. That change alone has helped doctors think differently about treatment.
What to Do Next
If you’ve been coughing for more than eight weeks:
- Stop any ACE inhibitor medication (if you’re on one) and talk to your doctor about alternatives.
- Get a chest X-ray and spirometry done. Don’t skip these.
- Try a 2-week trial of a first-gen antihistamine + decongestant (like chlorpheniramine + pseudoephedrine).
- If no improvement, try an inhaled steroid for 4 weeks.
- If still no change, try a high-dose PPI twice daily for 8 weeks.
- Keep a cough diary: note when it happens, what triggers it, and how bad it is.
Most people see improvement within 4 to 8 weeks. If not, ask about referral to a pulmonologist or allergist. There are new tools, new drugs, and better understanding than ever before.
Final Thought
A chronic cough isn’t just annoying-it can ruin sleep, make you exhausted, and even cause incontinence or cracked ribs. But it’s rarely a mystery. With the right steps, most people find relief. You don’t need a dozen tests or expensive scans. You need a smart, step-by-step approach. Start with the big three. Be patient. And don’t give up.
Can chronic cough be caused by something other than GERD, asthma, or postnasal drip?
Yes, but it’s uncommon. About 10% to 30% of chronic cough cases don’t respond to treatment for the three main causes. Other possibilities include chronic refractory cough (where nerves in the throat are oversensitive), vocal cord dysfunction, aspiration (inhaling food or liquid into the lungs), pertussis (whooping cough), or even side effects from certain medications like ACE inhibitors. Rare causes like lung cancer or tuberculosis are usually ruled out early with a chest X-ray and physical exam.
Why do some people with GERD not have heartburn but still have a cough?
This is called silent reflux. In these cases, stomach acid doesn’t travel far enough to cause burning in the chest. Instead, it reaches the throat or voice box and irritates sensitive nerves that trigger coughing. These people often feel a tickle in the throat, need to clear their throat often, or have a lump-like sensation. They might not even realize they have reflux until their cough improves after treatment.
Do antihistamines really help with postnasal drip cough?
Yes-but only first-generation ones like chlorpheniramine or diphenhydramine. They work because they cross into the nervous system and calm the cough reflex in the throat. Second-generation antihistamines like cetirizine or loratadine don’t work as well for cough because they don’t affect those nerves the same way. Adding a decongestant like pseudoephedrine boosts the effect, especially if nasal congestion is involved.
Is a chest CT scan necessary for chronic cough?
No, if your chest X-ray is normal. A CT scan exposes you to radiation equivalent to 74 chest X-rays and only finds cancer in about 0.1% of cases when the X-ray is clear. Guidelines from the European Lung Foundation and others strongly advise against routine CT scans. They’re only recommended if there are red flags like weight loss, coughing up blood, or abnormal findings on X-ray.
How long should I try a treatment before deciding it’s not working?
It depends on the treatment. For upper airway cough syndrome (antihistamines + decongestants), give it 1 to 2 weeks. For asthma (inhaled steroids), try 2 to 4 weeks. For GERD (PPIs), you need 4 to 8 weeks. Coughs don’t respond like infections-they take time. Stopping too soon can make you think the treatment didn’t work when it actually did. Keep a diary of your cough frequency and severity to track progress.