Every year, thousands of patients in the U.S. receive the wrong medication-not because of a doctor’s mistake, not because of a nurse’s oversight, but because two pills look too much alike on the shelf. One bottle says hydralazine, another says hydroxyzine. One label reads DOPamine, another DoBUTamine. To the untrained eye, they’re nearly identical. And in a busy pharmacy, where staff are juggling dozens of prescriptions at once, that tiny difference can be deadly.
This isn’t rare. According to the Institute for Safe Medication Practices (ISMP), about 18% of all medication error reports involve look-alike or sound-alike (LASA) drugs. That’s roughly 10,000 incidents annually. And it’s not just names. Packaging plays a huge role. Similar colors, fonts, bottle shapes, and label layouts make it easy to grab the wrong thing-even for experienced pharmacists.
Why This Problem Still Exists
Look-alike packaging confusion isn’t new. The Joint Commission flagged it as a national patient safety goal back in 1999. But despite decades of awareness, the problem persists. Why? Because many pharmacies still rely on human memory and visual scanning to pick drugs. And humans aren’t good at spotting tiny differences under pressure.
Consider this: a retail pharmacist might fill 80 prescriptions in a single shift. In that rush, they grab a bottle from a crowded shelf. The label is the same size. The font is the same. The color scheme? Identical. The only difference? One letter. In uppercase. Hidden in the middle of a long word. That’s not a design flaw-it’s a recipe for disaster.
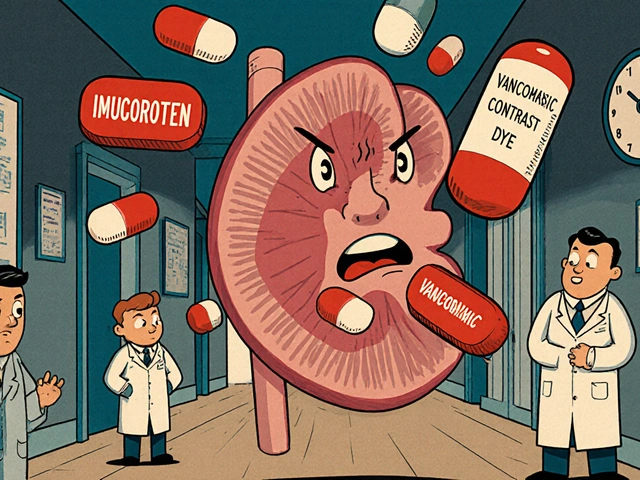
And it’s not just community pharmacies. Hospitals face the same issue. Insulin vials, heparin syringes, sedatives, and antibiotics often come in near-identical packaging. One wrong dose can lead to cardiac arrest, respiratory failure, or death.
The Three Proven Strategies That Work
There’s no single fix. But when you combine three evidence-based strategies, error rates drop dramatically. Here’s what actually works.
1. Physical Separation: The Simplest, Most Effective Fix
Put look-alike drugs far apart. Not just different aisles-different cabinets, different drawers, different shelves. The University of Arizona found this reduces errors by up to 62%. That’s not a small win. That’s life-saving.
It doesn’t require fancy tech. A simple plastic divider, a colored shelf tag, or even a sticky note saying “HIGH RISK-DO NOT GRAB WITHOUT DOUBLE-CHECK” can make a difference. One pharmacy in Arizona separated all insulin types into locked, labeled drawers. Within 18 months, wrong-insulin errors dropped from 3-4 per month to zero.
But here’s the catch: space is tight. Many pharmacies, especially small ones, don’t have room to spread everything out. That’s okay. You don’t need a whole new layout. Use existing storage wisely. Keep high-risk pairs like spironolactone and spiramycin on opposite ends of the same shelf. Use vertical space. Add risers. Use drawer dividers. Even $300 in shelf organizers can cut errors by half.
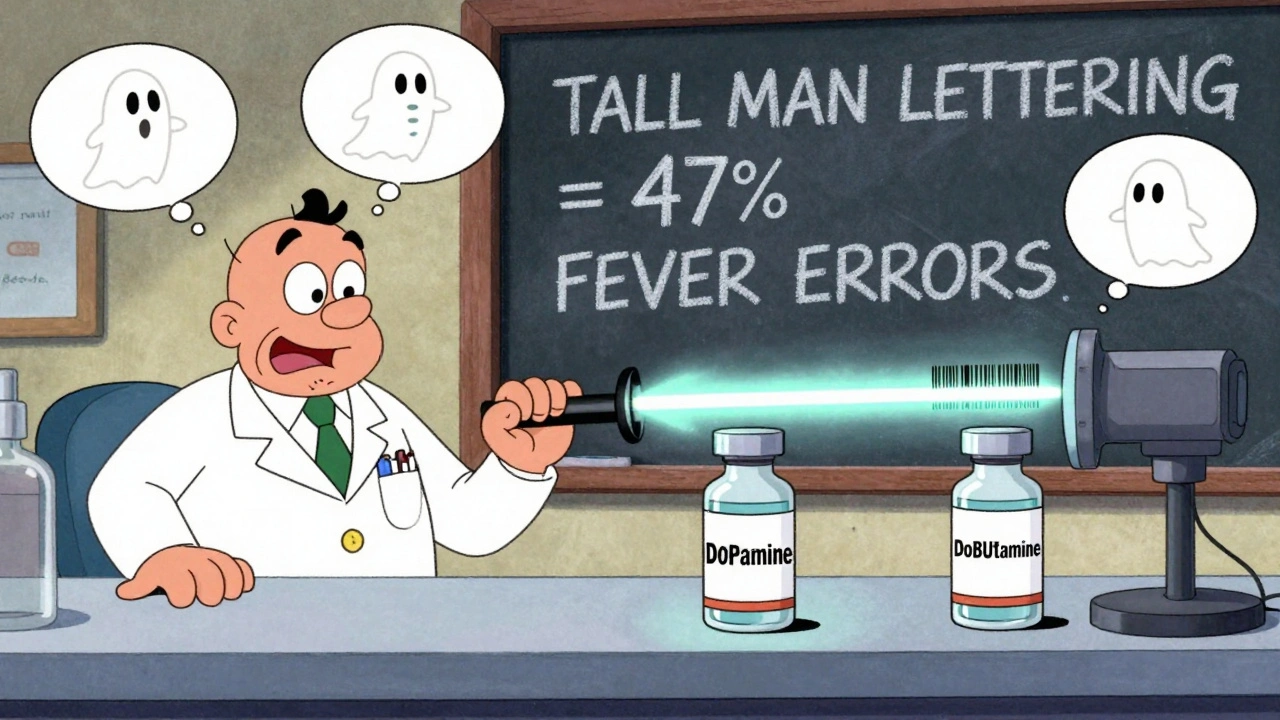
2. Tall Man Lettering: Make the Difference Visible
Tall Man Lettering (TML) isn’t a trick. It’s a visual cue. Instead of writing “dopamine” and “dobutamine,” you write DOPamine and DoBUTamine. The capital letters force your brain to pause and notice the difference.
ISMP’s research shows TML reduces selection errors by 47%. The FDA recommends it for over 100 high-risk drug pairs. And it’s free-once your pharmacy system supports it.
But here’s where it breaks down: not all systems do it right. Some EHRs only apply TML to the name on the screen. Others don’t print it on the label. One pharmacist in Ohio told us they spent weeks troubleshooting because the label printer ignored TML settings. The fix? Work with your vendor. Ask for a custom print template. Test it. Print a sample. Make sure the uppercase letters show up on the final label.
And don’t forget new drugs. Every time a new medication arrives, check if it looks or sounds like anything already in stock. ISMP updates its list of confused drug pairs quarterly. In January 2024, they added 17 new pairs-including buprenorphine and butorphanol. If you’re not checking, you’re not protected.
3. Barcode Scanning: The Last Line of Defense
Barcode scanning is the most powerful tool. When a pharmacist scans the drug, the system checks it against the prescription. If it doesn’t match? It alerts them. Immediately.
The Agency for Healthcare Research and Quality (AHRQ) found barcode scanning reduces administration errors by 86%. That’s the biggest single improvement you can make.
But here’s the problem: people bypass it. Nurses swipe the barcode without looking. Pharmacists scan the wrong bottle. One study at UC San Francisco found 5-12% of scans were skipped or done incorrectly.
The fix? Make scanning mandatory. Tie it to your workflow. No scan? No release. Add a checklist. Train staff to treat it like a seatbelt-something you do without thinking. And monitor compliance. Track how often scans are skipped. Reward teams that get it right 99% of the time.
What Doesn’t Work (And Why)
Some pharmacies try to solve this with posters. Or mnemonics. Or “be more careful.”
That’s not enough.
Dr. David Bates from JAMA Internal Medicine put it bluntly: “Over-reliance on Tall Man Lettering creates a false sense of security.” Why? Because TML only fixes name confusion. It doesn’t fix packaging. Two bottles can still look identical-even if the names are in different cases.
And staff education alone? It helps, but it’s not reliable. People get tired. They get distracted. They’re human. Systems should protect them-not expect them to be perfect.
How to Get Started Today
You don’t need a million-dollar budget. Start small. Here’s how.
- Do a quick LASA audit. Grab ISMP’s free Tool for Evaluating the Risk of Confusion Between Drug Names. Spend 2 hours listing your top 10 most confusing pairs. Common ones: clonidine and clonazepam, fluoxetine and fluvoxamine, hydroxyzine and hydralazine.
- Separate the top 3. Move them to different shelves or drawers. Use colored tape or labels. No cost. Immediate impact.
- Check your EHR. Does it use Tall Man Lettering on labels? Print a sample. If not, contact your vendor. Ask for a custom template. Demand it.
- Enforce barcode scanning. If you have scanners, use them. If you don’t, prioritize getting them. Even a basic handheld scanner costs under $200. The ROI? One prevented error pays for it ten times over.
- Create a daily checklist. Add “Verify LASA drugs” to your shift handover. Make it part of the routine.

What’s Coming Next
The FDA just released draft guidelines in February 2024 requiring standardized Tall Man Lettering for 25 new high-risk drug pairs. The National Council for Prescription Drug Programs (NCPDP) is building a universal LASA data format set to launch in late 2025. That means in a few years, every pharmacy system will automatically flag look-alike drugs-no manual work needed.
Meanwhile, AI is stepping in. Pilot programs at Johns Hopkins use machine learning to scan packaging images and flag potential look-alikes before a drug even hits the shelf. Accuracy? 98%.
This isn’t science fiction. It’s the future. And it’s coming fast.
Final Thought: Safety Is a System, Not a Wish
Preventing look-alike packaging errors isn’t about being more careful. It’s about designing systems that make mistakes nearly impossible.
Physical separation. Tall Man Lettering. Barcode scanning. These aren’t optional upgrades. They’re the bare minimum. And if your pharmacy isn’t using all three, you’re gambling with lives.
One wrong pill can end a life. But one smart system can save thousands.





Comments
Keasha Trawick
December 14, 2025
Let’s be real-this isn’t just about pharmacy errors. It’s about how we treat human cognition like a glitch to be fixed, not a feature to be respected. We design systems that assume people are robots, then punish them when they’re not. Tall Man Lettering? Sure. But if your shelf is a nightmare of 300 identical bottles, no amount of capital letters will save you. We need to stop romanticizing ‘being careful’ and start designing for distraction. Humans don’t fail because they’re lazy-they fail because the system is designed to make them fail.
Jamie Clark
December 15, 2025
You people are so obsessed with ‘systems’ you ignore the real problem: lazy management. If your pharmacy can’t afford $300 in shelf dividers, you shouldn’t be handling meds. This isn’t rocket science. It’s basic logistics. I’ve seen rural clinics with less than 10 staff do this right. It’s not about money-it’s about will. And if your boss doesn’t care enough to prevent a patient death, fire them. Or quit. Either way, stop pretending this is complicated.
Deborah Andrich
December 17, 2025
I’ve been a pharmacy tech for 14 years. I’ve almost grabbed hydralazine instead of hydroxyzine twice. Both times, I caught myself because the bottle felt slightly heavier. Not because of the label. Because of the damn bottle shape. We need to standardize packaging by weight and texture too. Not just letters. Think about blind pharmacists. Think about tired ones. Think about the ones who’ve been on their feet for 12 hours. Safety isn’t a checklist. It’s empathy built into design.
Sheldon Bird
December 18, 2025
Love this breakdown. Seriously. The barcode thing? Game changer. I work in a hospital and we started requiring scans for ALL high-risk meds last year. Errors dropped by 70% in 6 months. And yes, people still try to bypass it. So we added a little chime that plays when a scan fails. Sounds like a cartoon ‘ding!’ and it makes everyone laugh. But they never skip it anymore. 😄 Small wins matter.
Tommy Watson
December 18, 2025
why do we even have to do all this? like… cant we just tell people to read the labels? its not that hard. i mean come on. its one letter. how do you mess that up? also barcode scanners are so 2010. we got ai now. just point your phone at the bottle and let the phone do the work. lol
sharon soila
December 18, 2025
Thank you for writing this with such clarity. I’ve worked in community pharmacies for over two decades. The most powerful change I’ve seen? Physical separation. Not fancy tech. Not training. Just moving two bottles apart. One pharmacy I worked at put all the ‘-zine’ drugs on the top shelf, and all the ‘-zole’ on the bottom. No one had to remember anything. They just reached. And no one made a mistake. Simple. Human. Effective.
Constantine Vigderman
December 20, 2025
OMG this is so true!! I just saw a video of a nurse grabbing the wrong insulin and it made me cry 😭 We’re not asking for perfection-we’re asking for systems that don’t make us play Russian roulette with someone’s life. Barcode scanning isn’t optional. It’s the bare minimum. And if your pharmacy doesn’t have it? Tell them to get it. Now. Your neighbor could be next. 💪
Karen Mccullouch
December 20, 2025
Why are we letting foreign companies design our drug packaging? Look at this-half these drugs are made by EU or Asian labs that don’t even use Tall Man Lettering. We’re letting global supply chains dictate our patient safety. This isn’t a pharmacy problem. It’s a national security issue. We need American-made packaging standards. And we need them yesterday. 🇺🇸
nithin Kuntumadugu
December 21, 2025
ai scanning? lol. you think they dont track you? every time you scan a barcode, your data goes to big pharma. they know what meds you take. they sell it. this is all a control system. tall man lettering? its just to make you think you’re safe while they monitor you. and those ‘free’ ismp tools? they’re paid for by drug companies. nothing is free. nothing is safe. 🤖👁️
Cole Newman
December 22, 2025
bro you missed the real solution: color code everything. red for high risk, green for low, blue for weird ones. simple. intuitive. no brain needed. also why are we still using paper labels? just print the damn name in 72pt font with a neon outline. done. also why is this even a thing? why do these drugs even exist with names this similar? someone should get fired.
Bruno Janssen
December 24, 2025
I used to work in a pharmacy. I saw a man die because someone grabbed the wrong vial. I don’t talk about it. I just check every bottle three times now. I don’t care if it takes longer. I don’t care if the line gets long. I don’t care if they call me slow. I’d rather be late than responsible for someone’s funeral. I don’t need a system. I just need to remember. And I do.
Write a comment