When you’re diagnosed with IgA Nephropathy, the first question isn’t about symptoms-it’s about what happens next. Will your kidneys fail? Can you stop it? And is there real hope beyond just taking blood pressure pills? The answer has changed dramatically since 2025, thanks to a major update in global guidelines that rewrote how doctors treat this disease. IgA Nephropathy, also called Berger’s disease, isn’t rare. It’s the most common cause of primary glomerulonephritis worldwide, affecting 2.5 to 3.5 people per 100,000 each year-and up to 10 per 100,000 in parts of Asia. For many, it starts with a cold or sore throat, followed by dark, tea-colored urine. But for others, it shows up quietly during a routine blood test, with protein leaking into the urine and kidney function slowly dropping. The scary part? Up to half of those with persistent proteinuria will lose kidney function within 10 to 20 years. But now, that’s no longer inevitable.
What’s Really Driving Kidney Damage in IgA Nephropathy?
It’s not just high blood pressure or protein in the urine. Those are symptoms, not the root cause. The real problem is a faulty immune response. Your body makes abnormal forms of immunoglobulin A (IgA), which clump together with other proteins and get stuck in the filtering units of your kidneys-the glomeruli. This triggers inflammation, scarring, and gradual loss of kidney function. Think of it like rust forming inside a water filter. The filter doesn’t break all at once. It clogs slowly, piece by piece. That’s why early intervention matters so much.
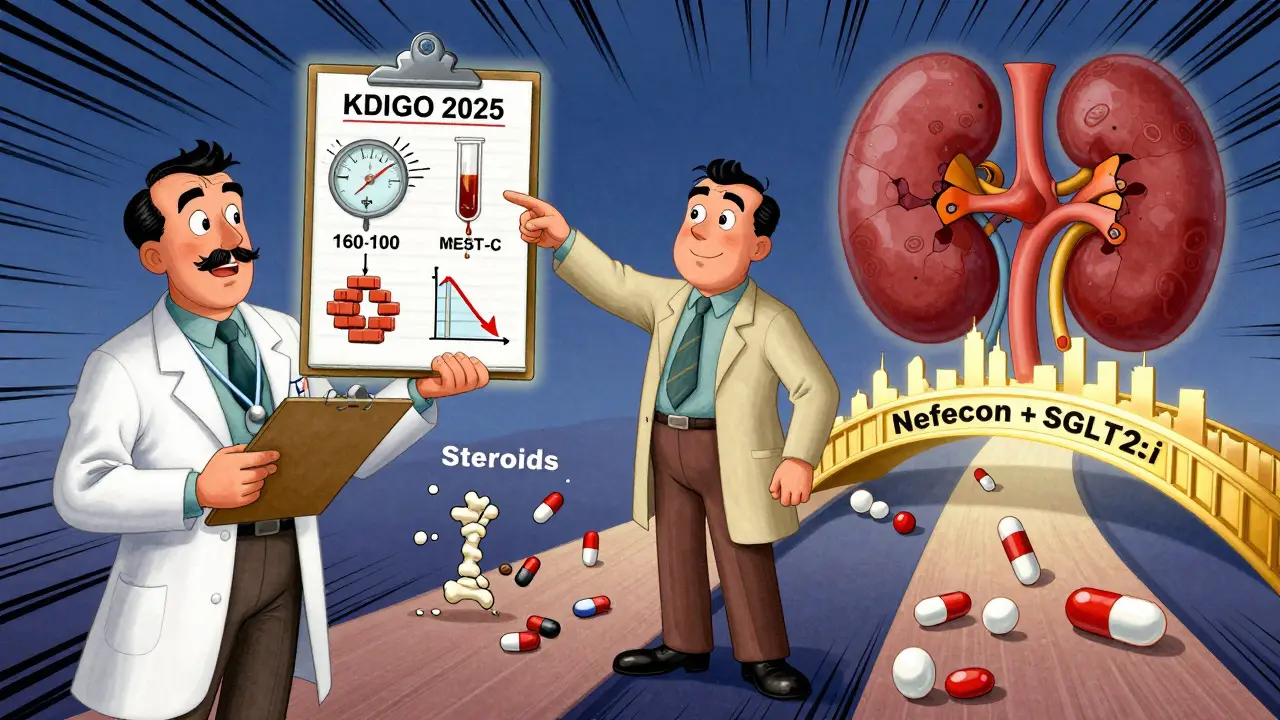
For years, treatment was passive: control blood pressure, reduce proteinuria, wait, and hope. But that approach let the disease keep ticking away during the waiting period. Now, we know that delaying treatment for 90 days-once standard practice-means losing more kidney tissue than necessary. The KDIGO 2025 guidelines flipped that script. They no longer recommend waiting. Instead, they push for immediate, combined therapy targeting both the immune trigger and the kidney’s response to injury.
The New Treatment Strategy: Two Fronts, One Fight
The KDIGO 2025 guidelines don’t just update drugs-they redefine the entire goal. The old target was proteinuria under 1 gram per day. The new target? Less than 0.5 grams per day. Why? Because data from kidney registries show that even patients with proteinuria between 0.44 and 0.88 g/g still had a 30% chance of reaching kidney failure within 10 years. That’s not safe. That’s a warning sign.
Today’s treatment has two parallel tracks:
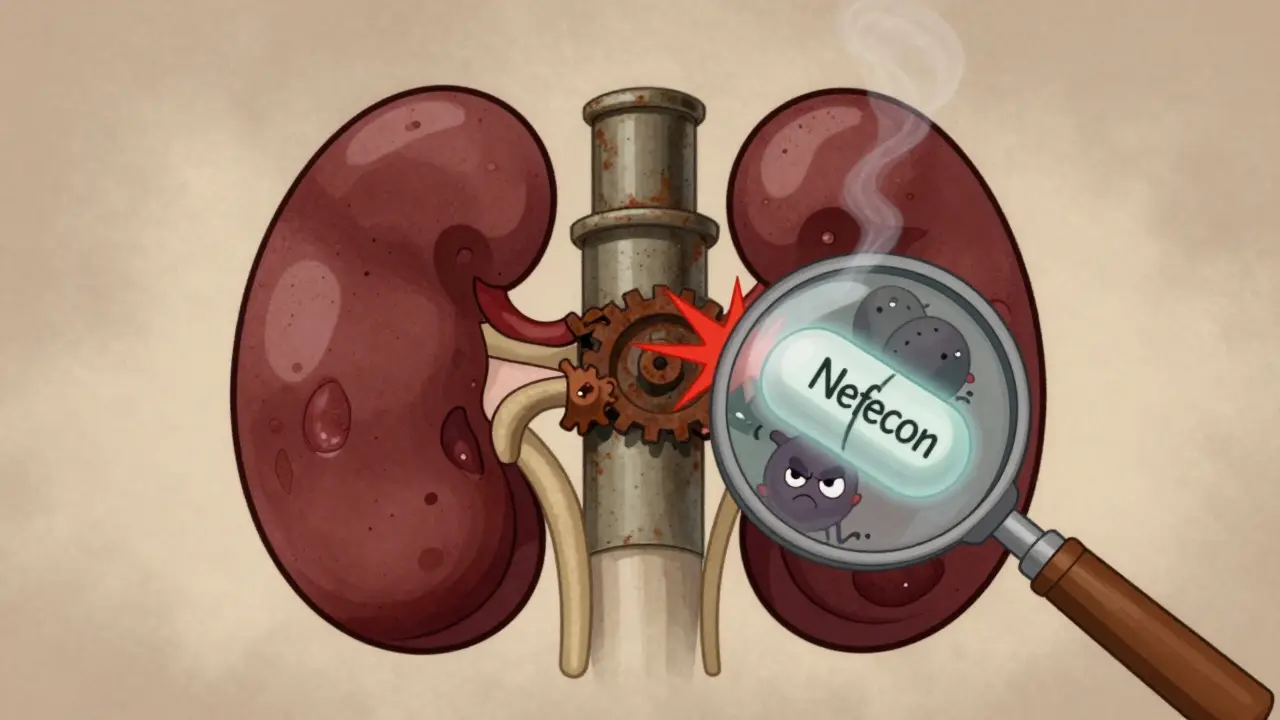
- Stop the immune attack: Block the production of bad IgA and stop it from damaging the kidneys. This is where new drugs like Nefecon come in. Nefecon is a targeted-release steroid that works in the gut-where IgA is made-instead of flooding your whole body. It reduces the abnormal IgA production at the source, with fewer side effects than traditional steroids. In trials, it cut proteinuria by over 50% in high-risk patients.
- Protect the kidneys from damage: Even if the immune system keeps firing, you can shield the kidneys. This is done with drugs that lower pressure inside the glomeruli: RAS inhibitors (like lisinopril or losartan), SGLT2 inhibitors (like dapagliflozin), and now sparsentan, a dual endothelin receptor antagonist. These drugs don’t just lower blood pressure-they directly reduce protein leakage and slow scarring.
For high-risk patients-those with proteinuria above 0.75 g/day and declining kidney function-the guideline now says: start both tracks at the same time. No waiting. No step-by-step. If you’re at risk, you get RASi + SGLT2i + Nefecon (or steroids) from day one.
What About Steroids? Are They Still Used?
Yes-but differently. Systemic steroids like prednisone were once the go-to immunosuppressant. But they come with weight gain, diabetes risk, bone loss, and mood swings. Many patients, especially teens and young adults, can’t tolerate them. That’s why Nefecon is a game-changer. In a 2025 patient survey of 150 people, 72% reported fewer side effects with Nefecon compared to oral steroids. Still, steroids aren’t gone. They’re reserved for patients who can’t access Nefecon or for those with severe inflammation on kidney biopsy. The trick now is choosing the right one for the right person.
Some regions still rely on older treatments. In Japan, tonsillectomy is common-up to 45% of patients get it, based on the theory that tonsils are a major source of bad IgA. In China, mycophenolate mofetil and hydroxychloroquine are frequently used. But these aren’t universally recommended. The KDIGO guidelines don’t endorse them outside specific populations because the evidence isn’t strong enough globally. What works in Tokyo might not work in Toronto.
How Do Doctors Know Who’s at Risk?
Not everyone with IgA Nephropathy needs aggressive treatment. That’s why risk stratification is now the first step. Doctors use a clinical calculator that looks at four things:
- Proteinuria level (the higher, the worse)
- Blood pressure (uncontrolled = higher risk)
- eGFR (how well kidneys filter-lower means more damage)
- Kidney biopsy results (using the Oxford MEST-C score, which rates scarring, cell growth, and other signs of injury)
If your proteinuria stays above 1 g/day after 3-6 months of blood pressure control, you’re high risk. Even if it’s between 0.75-1 g/day but your eGFR is dropping or your biopsy shows heavy scarring, you’re still in the high-risk group. That’s when combination therapy kicks in.
But here’s the catch: not every clinic is ready. A 2025 survey by the American Society of Nephrology found only 42% of U.S. nephrology practices had fully integrated the new risk tools into their electronic records. Many doctors are still using the old 2021 guidelines. If your doctor hasn’t mentioned the MEST-C score or Nefecon, ask why.
The Cost Problem: Can You Actually Get These Treatments?
Nefecon costs $125,000 a year in the U.S. Sparsentan isn’t cheap either. Insurance denials are common. One Reddit user, ‘IgAN_Mom,’ shared how her 16-year-old needed four medications, and insurance rejected Nefecon twice before a formal appeal worked. In the U.S., 68% of patients in online support groups reported initial denials. That’s not just a financial burden-it’s a delay that lets the disease progress.
The problem is global. In low- and middle-income countries, only 22% of patients get guideline-recommended care. Meanwhile, in high-income nations, 85% do. That’s a massive equity gap. Even if you’re in the U.S. or Europe, access depends on your insurance, your doctor’s network, and how aggressively you fight for coverage. Patient advocacy groups like the IgA Nephropathy Foundation are pushing for better access-but it’s slow.

What’s Coming Next? The Future of IgAN Treatment
The next five years will be transformative. Right now, 15 Phase 3 clinical trials are active. One, called TARGET-IgAN, is testing whether biomarkers can predict who will respond to which drug. Imagine a blood test that tells you: “You’ll respond to Nefecon but not steroids.” That’s the goal. Another trial is testing drugs that block APRIL, a protein that fuels bad IgA production. Vera Therapeutics and other biotechs are racing to bring these to market.
Dr. Jonathan Barratt, a leading nephrologist, predicts that within five years, treatment will be guided by biomarkers-not just protein levels or biopsy results. We’re moving from a one-size-fits-all model to precision medicine. But that also means complexity. More drugs, more tests, more decisions. And that’s where patient experience matters. The IgA Nephropathy Foundation’s 2024 survey found that 83% of patients care more about preserving quality of life than just slowing kidney decline. That’s why minimizing side effects is now as important as lowering proteinuria.
What Should You Do If You Have IgA Nephropathy?
Here’s what you need to do now:
- Get a full kidney biopsy if you haven’t already. The MEST-C score is critical.
- Ask for a proteinuria test using the urine albumin-to-creatinine ratio (UACR). Don’t settle for dipstick results.
- Request a calculation of your KDIGO risk score. If your doctor doesn’t know how, ask for a referral to a glomerular disease specialist.
- If you’re high risk, ask about Nefecon or sparsentan. Don’t assume steroids are the only option.
- Start an SGLT2 inhibitor if you’re not on one. Even if you don’t have diabetes, these drugs protect kidneys.
- Join a patient support group. Real stories from people living with IgAN help you navigate treatment fatigue and insurance battles.
It’s not about finding a cure. It’s about buying time-years, even decades-of healthy kidney function. And with today’s tools, that’s possible.
Can IgA Nephropathy be cured?
There is no cure for IgA Nephropathy yet. But with modern treatments, many patients can stop or significantly slow progression to kidney failure. The goal is long-term kidney protection, not elimination of the disease. Some patients achieve stable kidney function for decades with the right combination of therapies.
How long does it take for Nefecon to work?
Most patients see a drop in proteinuria within 3 to 6 months of starting Nefecon. Maximum effect usually occurs by 9 to 12 months. It’s not an instant fix-it’s a slow, steady reduction that builds over time. Regular urine tests every month for the first 3 months help track progress.
Is it safe to take SGLT2 inhibitors if I don’t have diabetes?
Yes. SGLT2 inhibitors like dapagliflozin and empagliflozin are now approved for kidney protection in people with chronic kidney disease-even without diabetes. They reduce proteinuria, lower blood pressure, and slow the decline of kidney function. Side effects like urinary tract infections or dehydration are possible but manageable with proper hydration and monitoring.
Why is proteinuria under 0.5 g/day the new target?
Research shows that even patients with proteinuria between 0.44 and 0.88 g/g still had a 30% risk of kidney failure within 10 years. The old target of 1 g/day was too high. Lowering proteinuria to under 0.5 g/day significantly reduces long-term risk. This is supported by large kidney registries and is now the standard in KDIGO 2025.
Should I get a tonsillectomy if I have IgA Nephropathy?
Tonsillectomy is not routinely recommended outside of Japan, where it’s widely used and supported by local studies. In Western countries, there isn’t enough evidence to prove it prevents kidney damage in most patients. If you’re considering it, ask your nephrologist whether your biopsy or IgA levels suggest a strong link between your tonsils and disease activity.
What if I can’t afford Nefecon or sparsentan?
If cost is a barrier, systemic steroids (like prednisone) combined with RAS inhibitors and SGLT2 inhibitors remain a valid, evidence-based option. Work with your doctor and a patient advocate to appeal insurance denials. Some drug manufacturers offer patient assistance programs. Never stop treatment because of cost-talk to your care team about alternatives.
What’s the Bottom Line?
IgA Nephropathy is no longer a waiting game. The tools to protect your kidneys are here. The challenge isn’t science-it’s access, awareness, and action. If you’ve been told to just monitor your blood pressure and wait, you’re being given outdated advice. The future of IgAN care is fast, targeted, and personalized. You deserve to know your real risk. You deserve to know your options. And you deserve to fight this disease with everything we now know works.




Comments
Ben McKibbin
January 21, 2026
Nefecon is a game-changer, but let’s be real - $125K a year is a joke. I’ve got a cousin on this drug, and his insurance fought him for 8 months. He’s 28, works at a coffee shop, and still got denied twice. The system isn’t broken - it’s designed to make you beg for your own kidneys. We need to stop treating kidney health like a luxury subscription.
Andrew Rinaldi
January 22, 2026
It’s fascinating how medicine has shifted from reactive to preemptive. We used to wait for the dam to break before we started patching it. Now we’re caulking the cracks before the first leak. The real victory isn’t just the drugs - it’s the mindset. Healing isn’t about fixing what’s broken anymore. It’s about protecting what’s still whole.
Glenda Marínez Granados
January 23, 2026
So let me get this straight - we now have a drug that targets IgA in the GUT… and we’re all supposed to be thrilled? 🤡 Next they’ll tell us to gargle with antibodies and call it a day. I mean, sure, it works - but why does it feel like we’re patching a sinking ship with duct tape and hope?
Write a comment