Methotrexate-NSAID Risk Calculator
This tool assesses the potential risk of kidney damage when taking methotrexate with NSAIDs based on medical guidelines. It is not a substitute for professional medical advice.
Important: Always consult your healthcare provider before combining these medications. This calculator provides general guidance only.
When you take methotrexate for rheumatoid arthritis or another autoimmune condition, you're counting on it to work safely. But add a common painkiller like ibuprofen or naproxen, and suddenly the risk isn't just about stomach upset-it's about your kidneys, your blood counts, and even your life. This isn't theoretical. It's happening in real patients, often because no one warned them.
How Methotrexate and NSAIDs Clash in the Kidneys
Methotrexate leaves your body through your kidneys. About 80% of it is cleared by the kidneys, mostly through active secretion in the tubules. NSAIDs-like ibuprofen, naproxen, and diclofenac-shut down prostaglandins, chemicals your kidneys need to keep blood flowing properly. When that happens, your kidneys get less blood. Less blood means less methotrexate gets filtered out.
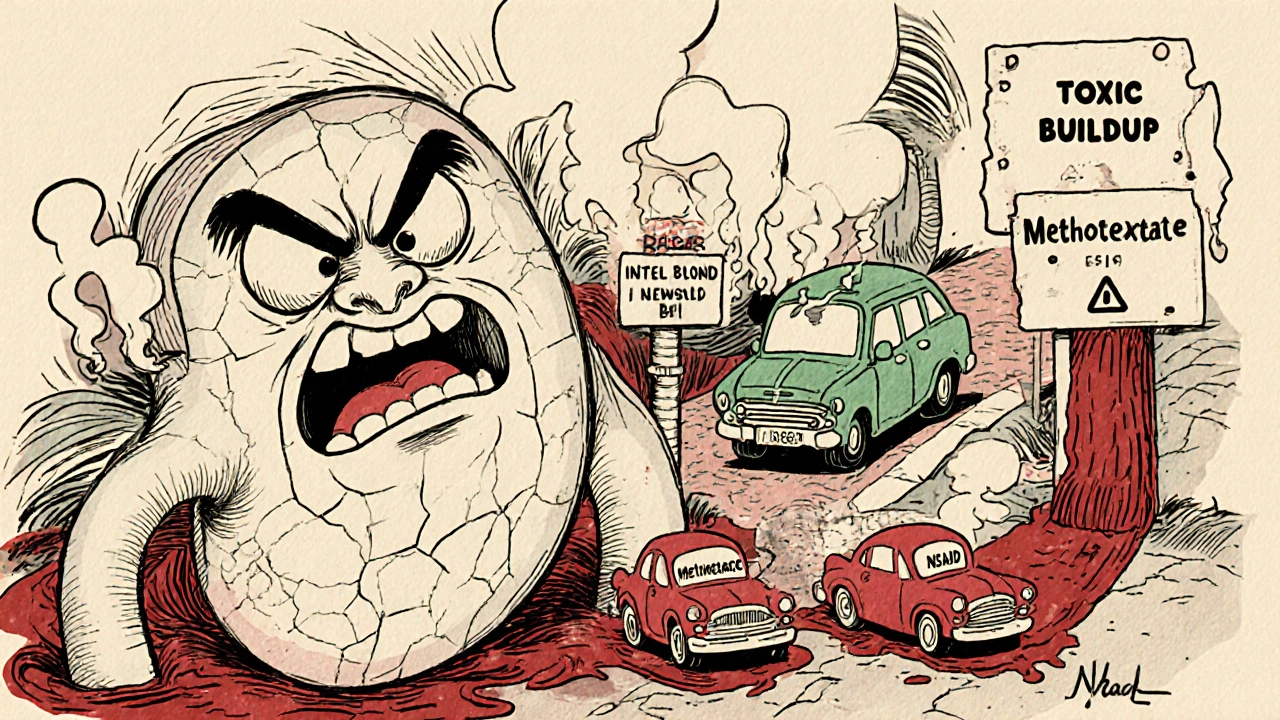
Studies show this interaction can reduce methotrexate clearance by 25% to 40%. That’s not a small drop. It means the drug builds up in your blood. At low doses (like 15 mg weekly for arthritis), this might just cause mild fatigue or nausea. But at high doses (used in cancer treatment), it can lead to life-threatening toxicity: bone marrow failure, severe infections, or acute kidney injury.
And it’s not just about blood flow. NSAIDs also compete with methotrexate for the same transporters in the kidney tubules. Think of it like two cars trying to get through a single toll booth. One gets stuck. That’s methotrexate. Meanwhile, NSAIDs can also knock methotrexate off proteins in your blood, freeing up more of the active drug to circulate. In lab tests, this increases free methotrexate levels by up to 30%.
High-Dose vs. Low-Dose: The Risk Isn’t the Same
The danger depends entirely on how much methotrexate you’re taking.
For cancer patients on high-dose methotrexate (500 mg/m² or more), combining it with NSAIDs is a red flag. A 2022 meta-analysis found these patients had a 4.7-fold higher risk of severe toxicity. Three fatal cases were reported to the FDA between 2018 and 2022. That’s why the EMA says NSAIDs should be avoided in high-dose therapy unless absolutely necessary-and even then, methotrexate levels must be checked every 24 hours for 72 hours.
For low-dose methotrexate (25 mg or less weekly), the picture is more mixed. One large 2019 study of over 4,000 rheumatoid arthritis patients found no significant increase in serious side effects when NSAIDs were used, as long as kidney function was normal. But here’s the catch: that study only looked at people with healthy kidneys. When researchers looked at patients with early kidney damage (eGFR between 45 and 59), the risk jumped. NSAID use increased the chance of hospitalization for kidney injury by 3.5 times.
That’s why experts disagree. Some say short-term, low-dose NSAIDs are okay if you’re monitored. Others say avoid them entirely if you’re over 65 or have any kidney issue. The truth? There’s no universal answer. It depends on your body, your dose, and your history.
Not All NSAIDs Are Created Equal
If you must take an NSAID, not all are equally risky.
Ketorolac is the worst offender. It’s a potent kidney blood flow reducer and can spike methotrexate levels by up to 50%. It’s rarely prescribed for long-term use, but it’s sometimes given in hospitals for severe pain-exactly when methotrexate patients are most vulnerable.
Ibuprofen and naproxen fall in the middle, increasing methotrexate levels by 25-30%. Diclofenac is similar. But celecoxib, a COX-2 selective NSAID, shows less interference. Studies suggest it raises methotrexate levels by only 10-15%. That’s not zero risk, but it’s the best option if you need an NSAID.
And don’t assume “natural” means safer. Willow bark, turmeric, or ginger supplements can also inhibit prostaglandins. They’re not regulated like drugs, but they can still interfere with methotrexate clearance.
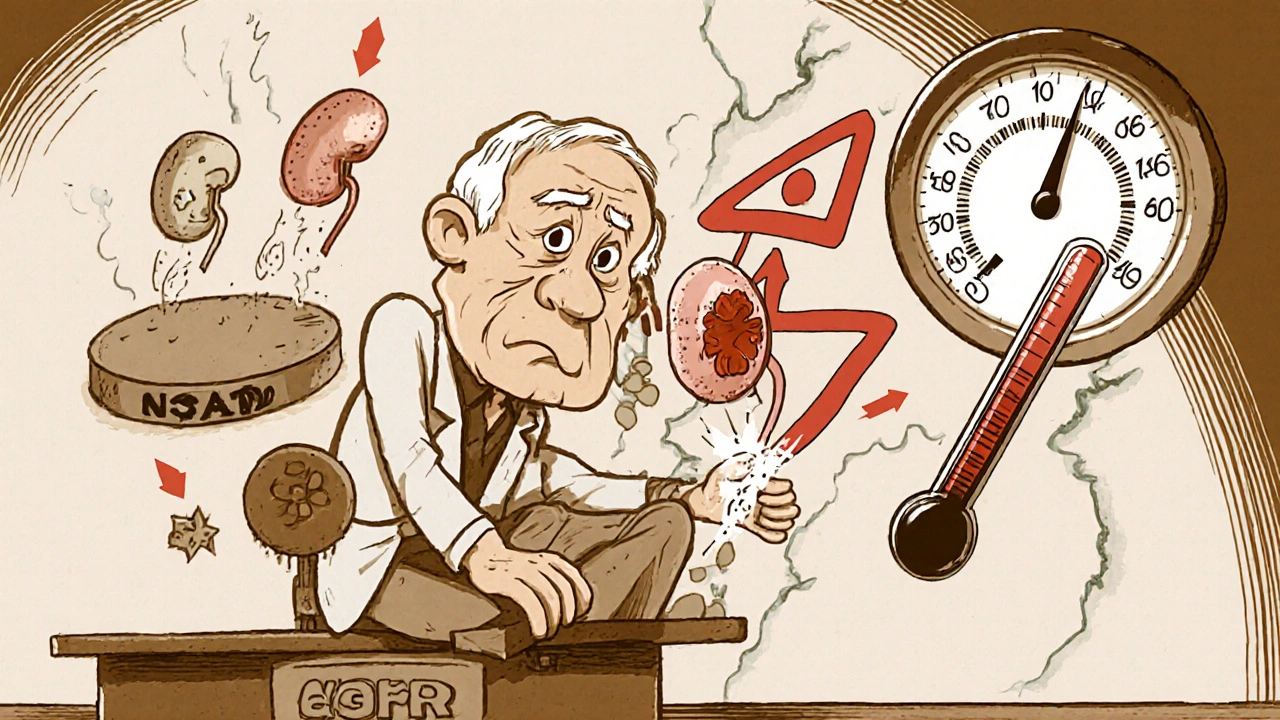
Who’s Most at Risk?
It’s not just about the drugs. Your body matters too.
- Age 65+: Kidneys naturally slow down. Even mild decline increases risk.
- eGFR under 60: Any sign of kidney trouble makes you vulnerable.
- Dehydration: Less fluid = less kidney flow = more drug buildup.
- Diabetes or high blood pressure: These damage kidneys over time, often silently.
- Genetics: About 15% of Caucasians carry a gene variant (SLC19A1 80G>A) that makes them absorb and retain methotrexate more easily. Add NSAIDs, and levels spike even more.
And here’s the scary part: most of these risks are silent. A 2020 review found 63% of kidney problems from this interaction showed no symptoms until blood tests revealed elevated creatinine. Patients felt fine-until they didn’t.
What the Experts Say
Dr. Joan Kremer from Thomas Jefferson University says: “We used to ban all NSAIDs with methotrexate. Now we know it’s not that simple. With monitoring, short-term use can be safe.”
But Dr. Daniel Furst from UCLA warns: “In older patients or those with any kidney change, the risk of death goes up nearly threefold. Avoid NSAIDs. Period.”
The FDA’s label now says NSAIDs may reduce methotrexate clearance and increase toxicity. The EMA went further: avoid NSAIDs in anyone on more than 10 mg/week of methotrexate unless absolutely necessary.
These aren’t just guidelines. They’re based on real deaths and hospitalizations.
What You Should Do
If you’re on methotrexate and need pain relief:
- Don’t start an NSAID without talking to your doctor. Even if it’s OTC.
- Get your kidney function tested. Ask for eGFR and serum creatinine. Do this before starting, and again 48-72 hours after.
- Check your blood counts. Methotrexate lowers white blood cells. NSAIDs can make that worse. A CBC should be done at the same time.
- Use the lowest dose for the shortest time. Three days of ibuprofen is safer than three weeks.
- Space out the doses. Take methotrexate in the morning, NSAID in the evening-12 hours apart reduces peak overlap.
- Consider alternatives. Acetaminophen (up to 3,000 mg/day) is generally safe. Physical therapy, heat, or low-dose opioids for short-term use are options too.
And if you’re on high-dose methotrexate for cancer? NSAIDs are usually off-limits. If pain is severe, your oncology team will use other strategies-hydration, leucovorin rescue, or non-NSAID pain meds.
Real Stories, Real Consequences
On Reddit, a user named ‘RAWarrior2020’ wrote: “My rheumatologist prescribed naproxen without checking my kidneys. Three days later, I was vomiting, exhausted, and my white blood cell count dropped to 1.8. I needed leucovorin to survive.”
Another user, ‘MTXandMe’, said: “I’ve taken methotrexate with ibuprofen for 8 years. No problems. But my doctor checks my labs every 4 weeks. That’s the difference.”
A 2022 Arthritis Foundation survey found that 41% of patients who took NSAIDs without monitoring had an adverse event. Only 9% did when labs were checked regularly.
Pharmacists who actively screen for this interaction have cut the rate of adverse events by 63%. That’s not magic. It’s just asking the right questions.
What’s Next?
Researchers are working on point-of-care devices that can measure methotrexate levels in minutes-like a glucose meter for this drug. Clinical trials are underway. In the future, your pharmacist might check your methotrexate level right after you pick up your NSAID.
Until then, the rules are simple: know your kidney function. Know your dose. Know your NSAID. And never assume a painkiller is harmless just because it’s over the counter.
Methotrexate saves lives. NSAIDs ease pain. But together, without caution, they can break your kidneys-and your body-without warning.





Comments
Patricia McElhinney
November 26, 2025
Methotrexate and NSAIDs? Please. I’ve been a clinical pharmacist for 22 years and I’ve seen this exact scenario kill people. You think ibuprofen is harmless? It’s not. The kidneys don’t care if it’s OTC. They just care about transporters and glomerular filtration. And if your eGFR is below 60? You’re playing Russian roulette with your bone marrow. The FDA label says it. The EMA says it. But no one listens until their creatinine hits 3.5 and they’re in the ICU. Stop being lazy. Get tested. Or don’t. But don’t blame your doctor when you’re on a ventilator because you thought ‘it’s just a pill’.
Agastya Shukla
November 26, 2025
From a pharmacokinetic standpoint, the competitive inhibition at OAT3 and RFC1 transporters is well-documented. The displacement of methotrexate from plasma proteins by NSAIDs further increases the free fraction, which is pharmacologically active. The AUC increase can reach 30–50% depending on the NSAID’s affinity. Celecoxib’s lower affinity for OAT3 explains its relatively safer profile. However, even a 10% elevation in plasma concentration can be clinically significant in patients with polymorphisms in SLC19A1. Monitoring serum levels, especially in those with eGFR <60, is not optional-it’s standard of care.
giselle kate
November 28, 2025
USA doctors are too soft. We let people take ibuprofen like candy. In my country, if you’re on methotrexate, you’re banned from NSAIDs. Period. No ‘maybe’, no ‘if your kidneys are fine’-you don’t get to gamble with your life. And don’t tell me about ‘natural’ remedies either. Turmeric? That’s just aspirin with a yoga pose. We don’t need American ‘balance’. We need discipline. Your kidneys aren’t a suggestion box. They’re your lifeline. Treat them like it.
Leisha Haynes
November 29, 2025
So you’re telling me I can’t take Advil for my arthritis pain while on methotrexate… but acetaminophen is fine? Cool. So basically my pain gets to be a side hustle while my meds try to kill my immune system. Thanks for the optimism. I’ll just sit here and cry into my Tylenol bottle like a good little patient. At least I’m not risking kidney failure… or maybe I am? Who knows. My doctor’s too busy to check labs every month anyway. 😌
Shivam Goel
December 1, 2025
Let’s be precise: NSAIDs inhibit COX-1 and COX-2, reducing PGE2 synthesis → vasoconstriction of afferent arterioles → decreased GFR → reduced methotrexate clearance. Concurrently, NSAIDs compete with methotrexate for renal tubular secretion via OAT1/OAT3. This is not a ‘risk’-it’s a biochemical inevitability. The 2019 study you cite? It excluded patients with eGFR <60-so it’s statistically irrelevant for the population most at risk. And celecoxib? Still inhibits COX-2, which regulates renal perfusion. ‘Safer’ is a misleading term. ‘Less dangerous’-yes. ‘Safe’-no. You’re not mitigating risk-you’re delaying the inevitable.
Andrew Camacho
December 2, 2025
Okay so here’s the thing-I’ve been on methotrexate for 11 years. I’ve taken ibuprofen for migraines since 2015. No hospitalizations. No crashes. My labs? Perfect. My doctor? He checks my CBC and creatinine every 6 weeks. So why are we acting like this is a death sentence? I get it-there are risks. But so is breathing. Life is risk. The real tragedy isn’t the drug interaction-it’s the fear-mongering. People are terrified of pills. But they’ll take 3 cups of coffee and 2 energy drinks a day. Tell me which one’s really killing you. This post reads like a horror movie trailer. Reality? It’s just medicine. With monitoring, you’re fine.
Arup Kuri
December 3, 2025
Big Pharma doesn’t want you to know this but NSAIDs are secretly designed to work with methotrexate so you need more pills. They profit from kidney failure. They profit from dialysis. They profit from bone marrow transplants. The FDA? Controlled by the same people who own the drug companies. That’s why they say ‘monitor’-not ‘avoid’. They want you to keep buying. And the ‘natural’ remedies? That’s a distraction. They want you to think ginger is dangerous so you’ll keep buying celecoxib. Wake up. Your kidneys are being slowly murdered by a system that profits from your suffering.
Elise Lakey
December 4, 2025
I’ve been on methotrexate for 6 years and I’ve never taken an NSAID. I use heat wraps, acupuncture, and gentle yoga. It’s not perfect, but I sleep better and I don’t worry about my kidneys. I know it’s not for everyone-but if you’re scared, you’re not alone. I was too. But learning to listen to my body, not just the pill bottle, changed everything. You don’t have to choose between pain and safety. There’s a middle path. It just takes patience.
Erika Hunt
December 5, 2025
I really appreciate how thorough this post is-it’s rare to see such a nuanced, evidence-based breakdown of a common but dangerous interaction. I’ve been reading up on this since my doctor mentioned the risk last month, and honestly, I was terrified. But now I feel more informed than scared. The part about SLC19A1 gene variants? That was new to me. I got tested last week-turns out I’m negative. That’s a huge relief. And I didn’t know celecoxib was less risky-I’m going to ask my pharmacist about switching. Thank you for not just saying ‘avoid everything’ but giving real, actionable steps. It makes a difference.
Shirou Spade
December 6, 2025
Every drug is a conversation between chemistry and biology. Methotrexate is a scalpel. NSAIDs are a blunt hammer. When you use them together, you’re not just treating pain-you’re disrupting a delicate equilibrium that took millions of years to evolve. The kidneys aren’t a filter. They’re a symphony. And when you jam one instrument into the score, the whole piece collapses. But here’s the paradox: we need pain relief. We need to live. So the answer isn’t purity-it’s awareness. The answer isn’t fear-it’s mindfulness. We don’t have to choose between healing and hurting. We just have to know what we’re doing.
Write a comment