PPI-Clopidogrel Interaction Checker
Check Your Medication Risk
Select your medications to see if there's a significant interaction that could reduce clopidogrel's effectiveness.
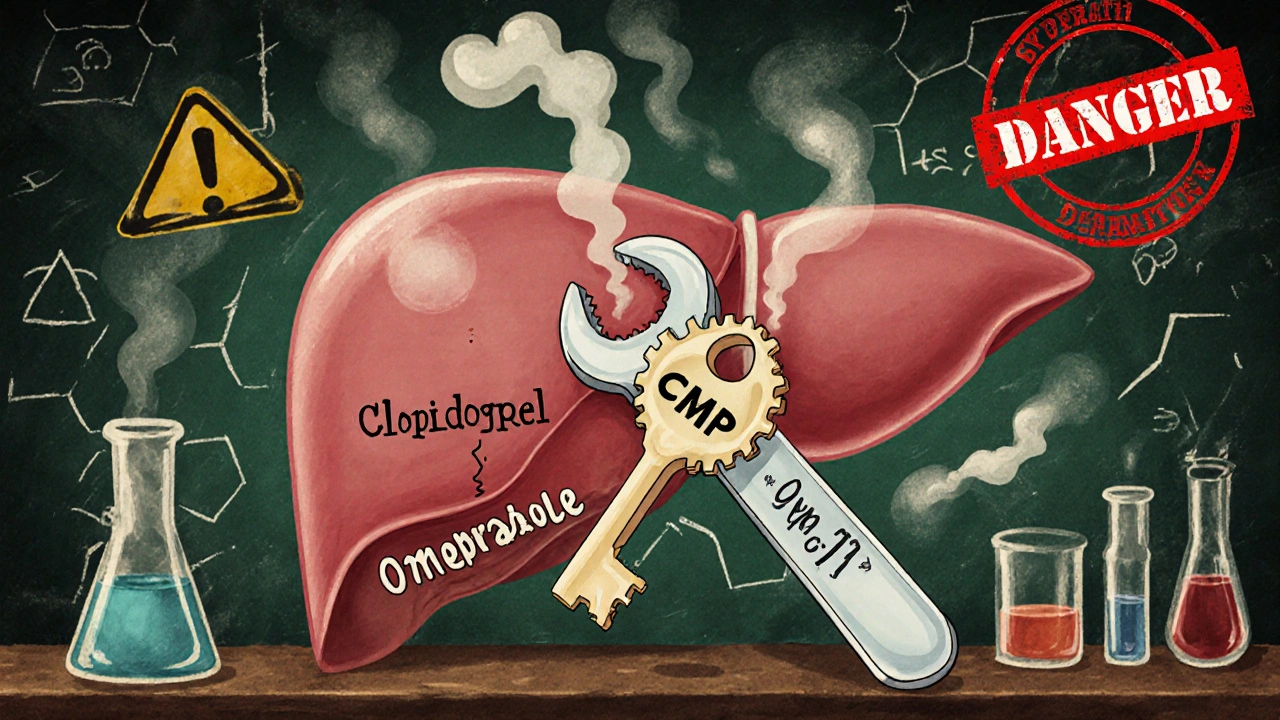
If you’re taking clopidogrel to prevent heart attacks or strokes, and your doctor also prescribed omeprazole for acid reflux or ulcers, you might be at risk for a hidden drug interaction-one that could reduce clopidogrel’s effectiveness by nearly half. This isn’t theoretical. It’s backed by clinical studies, regulatory warnings, and real-world data from over 270,000 patients. The culprit? A liver enzyme called CYP2C19.
How Clopidogrel Actually Works
Clopidogrel doesn’t work right away. It’s a prodrug, meaning your body has to turn it into something active before it can do its job. That job? Blocking platelets from clumping together and forming dangerous blood clots. The problem is, your liver needs to activate it using an enzyme called CYP2C19. Without this step, clopidogrel is basically useless.Think of it like a key that needs to be cut before it can unlock a door. Clopidogrel is the blank key. CYP2C19 is the machine that cuts it. If the machine is broken or blocked, the key doesn’t work-and your blood stays sticky.
Why Omeprazole Is the Problem
Omeprazole, a common proton pump inhibitor (PPI) used for heartburn and stomach ulcers, is also processed by CYP2C19. But here’s the catch: while it’s being broken down, it latches onto the enzyme so tightly that clopidogrel can’t get a turn. It’s like two people trying to use the same bathroom at the same time-one locks the door, and the other is stuck outside.Studies show that a daily 80mg dose of omeprazole reduces clopidogrel’s active metabolite by 45%. Even the standard 20mg dose cuts it by 32%. That’s not a small drop. That’s enough to weaken its ability to prevent clots. The FDA issued a safety warning in 2009 after data from Brandt (2007) and Sibbing (2008) showed this effect clearly. Since then, guidelines from the American Heart Association and European Society of Cardiology have told doctors to avoid combining these two drugs.
Not All PPIs Are Created Equal
Here’s where things get practical. Not every acid reducer messes with clopidogrel the same way. The strength of CYP2C19 inhibition varies widely across PPIs:- Omeprazole: Strongest inhibitor. Reduces clopidogrel’s active metabolite by up to 49% at high doses.
- Esomeprazole (the S-isomer of omeprazole): Almost as bad. About 40% reduction at 40mg daily.
- Lansoprazole: Mild effect at standard doses. Only 5% reduction in overall exposure, though high doses (60mg) can cut peak levels by 18%.
- Pantoprazole: Minimal inhibition. Only 14% reduction in clopidogrel exposure-even at 40mg. This makes it the safest PPI option if you absolutely need one.
- Rabeprazole: Slight reduction in peak levels (28%), but doesn’t affect total exposure. A reasonable alternative.
- Ilaprazole: Newer and weakest inhibitor. No significant effect on clopidogrel in recent studies (2025).
So if you’re on clopidogrel and need stomach protection, pantoprazole is your best bet. Rabeprazole is next. Omeprazole and esomeprazole? Avoid them.
Genetics Make It Worse
Your genes matter. About 30% of East Asians and 20-25% of Caucasians carry a genetic variant called CYP2C19*2 or *3. These are called loss-of-function alleles. They mean your liver is already slow at activating clopidogrel. Add omeprazole on top, and your active metabolite levels can drop by over 50%.A Korean study found that in people with normal CYP2C19 function, omeprazole reduced clopidogrel’s effect by 32%. But in those with the bad gene? It dropped by 54%. That’s not just a risk-it’s a recipe for a heart attack or stroke.
The Clinical Pharmacogenetics Implementation Consortium (CPIC) recommends that if you’re a poor or intermediate metabolizer and need a PPI, switch from clopidogrel to prasugrel or ticagrelor. These drugs don’t rely on CYP2C19. They’re more expensive, but they work reliably-even with acid meds.
But Do We Really See More Heart Attacks?
This is where the debate gets messy. On one hand, the numbers scream danger: a 2014 meta-analysis of 271,551 patients showed a 27% higher risk of heart attack or death when clopidogrel was taken with any PPI. Omeprazole alone raised the risk by 33%.On the other hand, the COGENT trial-a randomized, controlled study with 3,761 patients-found no difference in heart events between those taking omeprazole and those who didn’t. The FAST-MI Registry, tracking over 2,700 patients, also found no increased risk of cardiovascular events after one year.
Why the contradiction? Experts think it’s because many patients in observational studies were sicker to begin with. They had ulcers because they were already at high risk for clots. The PPI wasn’t causing the problem-it was just a marker of higher risk. Meanwhile, the COGENT trial excluded high-risk patients and used a low dose of omeprazole (10mg), which may not have been enough to trigger the interaction.
Timing Doesn’t Help
Some people think: “What if I take clopidogrel in the morning and omeprazole at night?” It sounds logical. But it doesn’t work. A 2013 study proved that separating the doses by hours doesn’t prevent the inhibition. CYP2C19 is a liver enzyme-it doesn’t care when you take the pills. It’s always there, and omeprazole lingers long enough to block it all day.
What Should You Do?
If you’re on clopidogrel and need a PPI:- Avoid omeprazole and esomeprazole entirely. They’re the worst offenders.
- Choose pantoprazole 40mg daily as your first option. It has the least interaction.
- Consider rabeprazole 20mg daily if pantoprazole isn’t available.
- Ask about H2 blockers like famotidine. They don’t affect CYP2C19 and are effective for many types of reflux.
- Ask your doctor about genetic testing for CYP2C19. If you’re a poor metabolizer, switch to ticagrelor or prasugrel.
Don’t stop your meds. But do talk to your doctor or pharmacist. This isn’t about fear-it’s about smart choices.
What’s Changing in 2025?
New research is making this clearer. The 2025 Nature Scientific Reports study confirmed ilaprazole has the weakest CYP2C19 inhibition of all PPIs-so far, no effect on clopidogrel. It’s not yet widely available, but it’s a sign of where things are headed.The FDA’s 2023 draft guidance now uses a more precise model called the R-value to predict drug interactions. An R-value over 1.25 means clinical concern. Omeprazole scores 1.5-1.8. Pantoprazole? Just 1.1. That’s the kind of science guiding future prescribing.
And cardiology practices are catching up. According to the American College of Cardiology’s 2023 registry, 74% of clinics now use some form of CYP2C19 testing for patients on clopidogrel who need acid control. Personalized medicine isn’t the future anymore-it’s here.
Bottom Line
Omeprazole and clopidogrel don’t mix well. The science is solid: omeprazole blocks the enzyme clopidogrel needs to work. The clinical impact is debated, but the risk is real-especially if you have the genetic profile that makes you a slow metabolizer.You don’t need to avoid all PPIs. You just need to avoid the wrong ones. Pantoprazole works. Rabeprazole works. Omeprazole? Don’t risk it.
If you’re on both, talk to your doctor. Ask about your CYP2C19 status. Ask about alternatives. Your heart might depend on it.
Can I take omeprazole with clopidogrel if I take them at different times of day?
No. Separating the doses-like taking clopidogrel in the morning and omeprazole at night-does not prevent the interaction. Both drugs are processed by the same liver enzyme (CYP2C19), and omeprazole stays in your system long enough to block it all day. Studies have confirmed this. Timing doesn’t help.
Is pantoprazole safe to take with clopidogrel?
Yes. Pantoprazole has the weakest effect on CYP2C19 among all PPIs. Clinical studies show it reduces clopidogrel’s active metabolite by only about 14%, which is not considered clinically significant. Major guidelines, including those from the American College of Gastroenterology, recommend pantoprazole as the preferred PPI for patients on clopidogrel.
Why is omeprazole more dangerous than other PPIs with clopidogrel?
Omeprazole binds to the CYP2C19 enzyme with much higher affinity than other PPIs. Its inhibition strength (IC₅₀ of 2-4 μM) is the strongest among all proton pump inhibitors. It also has a Cmax,u/Ki,u ratio of 0.04-0.06, which exceeds the FDA’s threshold (≥0.02) for clinically relevant inhibition. Other PPIs like pantoprazole and rabeprazole fall well below this level.
Do I need genetic testing if I’m on clopidogrel?
If you’re on clopidogrel and need a PPI, yes-genetic testing for CYP2C19 is strongly recommended. About 30% of people have genetic variants that make them poor or intermediate metabolizers. For them, omeprazole can reduce clopidogrel’s effect by over 50%. Testing helps identify those at highest risk and guides safer choices, like switching to ticagrelor or prasugrel.
What are the alternatives to clopidogrel if I need a PPI?
If you need long-term acid suppression and are a poor metabolizer of CYP2C19, prasugrel and ticagrelor are better options. Unlike clopidogrel, they don’t rely on CYP2C19 to become active. They work faster, are more consistent, and aren’t affected by PPIs. They’re more expensive, but for high-risk patients, the benefit outweighs the cost.
Is there a PPI that doesn’t interfere with clopidogrel at all?
Ilaprazole, a newer PPI, shows the weakest inhibition of CYP2C19 in recent studies (2025). Clinical trials found no significant effect on clopidogrel’s antiplatelet activity. However, it’s not yet widely available outside parts of Asia. Until it’s approved elsewhere, pantoprazole remains the safest and most accessible choice.
Can I use famotidine instead of a PPI with clopidogrel?
Yes. Famotidine is an H2-receptor antagonist, not a PPI. It reduces stomach acid through a different mechanism and does not inhibit CYP2C19. It’s a good alternative for patients on clopidogrel who need gastric protection but can’t use omeprazole or esomeprazole. It’s less potent than PPIs for severe ulcers, but effective for most cases of heartburn and mild reflux.




Comments
Shana Labed
October 31, 2025
OMG I just found out my doc gave me omeprazole with my clopidogrel and I’ve been taking it for 8 months 😱 I’m so glad I saw this post-went straight to my pharmacist and they switched me to pantoprazole same day. My heart’s gonna thank me later. Y’all need to check your meds ASAP-this isn’t hype, it’s survival.
California Daughter
October 31, 2025
Wait… so you’re saying… that… the FDA… warned… about this… in… 2009… and yet… people… are… still… getting… prescribed… omeprazole… with… clopidogrel…? Like… are… doctors… just… not… reading…? Or… is… this… a… pharma… conspiracy…? I… need… a… flowchart…
Vishwajeet Gade
October 31, 2025
bro u guys are overthinking this. in india we take omeprazole with clopidogrel daily. no problem. your system is weak. eat more spicy food. no need for pantoprazole. just chill.
Casey Crowell
November 1, 2025
Just had my CYP2C19 test done last month-turns out I’m a poor metabolizer 😅 So yeah, I switched from clopidogrel to ticagrelor. Worth every penny. My cardiologist said, 'You’re not just saving money-you’re saving your life.' And honestly? I cried a little. This stuff matters. 🫂
Shanna Talley
November 2, 2025
Thank you for writing this. So many people are scared to ask their doctors questions. But if you’re on clopidogrel and have heartburn, just say: 'Can we try pantoprazole instead?' It’s simple. It’s safe. And it might save your life. You’ve got this.
Samuel Wood
November 2, 2025
Actually, the 2025 Nature study you cited? It’s a preprint. Not peer-reviewed. And you’re ignoring the COGENT trial’s null result. This whole narrative is fearmongering dressed up as science. Also, 'ilaprazole'? That’s not even FDA-approved. You’re giving false hope.
Jacqueline Anwar
November 4, 2025
It is deeply concerning that such a well-documented pharmacokinetic interaction continues to be ignored by primary care physicians. The clinical implications are not merely theoretical-they are quantifiable, reproducible, and catastrophic. One must question the integrity of contemporary medical education when such foundational knowledge is disregarded.
Ganesh Kamble
November 4, 2025
pantoprazole? lol. why not just take TUMS? cheaper, no interaction, and you don't need a PhD to understand it. also, why are you all so scared of acid? your stomach is fine.
Jenni Waugh
November 5, 2025
Ohhh so now we’re playing doctor because someone wrote a blog? Let me guess-you also think vaccines cause autism and 5G is mind control. This isn’t 'personalized medicine,' it’s alt-med with a fancy acronym. Next you’ll be recommending turmeric for stents.
Theresa Ordonda
November 6, 2025
My mom died of a stroke last year. She was on clopidogrel and omeprazole for 3 years. I didn’t know this was a thing until now. I’m furious. Not at you. At the system. How many people are dying because doctors don’t check drug interactions? 😭
Judy Schumacher
November 6, 2025
So… you’re saying… I’ve been taking omeprazole with clopidogrel for 5 years… and… I’m… a… slow metabolizer… and… now… you’re telling me… I… should’ve… been… on… ticagrelor… since… day… one…? And… my… cardiologist… never… mentioned… this…? And… I’m… still… alive…? So… what… was… the… point… of… all… this…?
Megan Raines
November 8, 2025
So… what’s the deal with famotidine? I’ve been taking it for years. Is it really safe? Or am I just lucky?
Mamadou Seck
November 9, 2025
pantoprazole is fine but if you want real relief just drink apple cider vinegar. no science just vibes. also i took omeprazole with clopidogrel for 2 years and i’m still here so chill
Anthony Griek
November 10, 2025
My dad’s on clopidogrel and he’s been taking pantoprazole for 4 years. No issues. No heart attacks. Just regular checkups. I think this whole thing is blown way out of proportion. People need to stop panicking and start talking to their doctors.
Norman Rexford
November 11, 2025
Look I’m not saying you’re wrong… but… what if… the real problem… is… that… we’re… all… just… too… medicated…? Like… why do we even need PPIs? Maybe we should just eat less pizza… and… sleep better… and… stop… stressing… about… everything…? Just… a… thought… 🤔
Write a comment