When you take an opioid for severe pain-after surgery, a broken bone, or cancer treatment-it works fast and well. But what happens when that relief becomes harder to get? Or when stopping feels impossible? And why do some people die from an overdose even after years of use, while others die after just one relapse? The answers lie in three hidden processes: tolerance, dependence, and overdose. These aren’t just side effects. They’re biological shifts that can turn a helpful medicine into a life-threatening cycle.
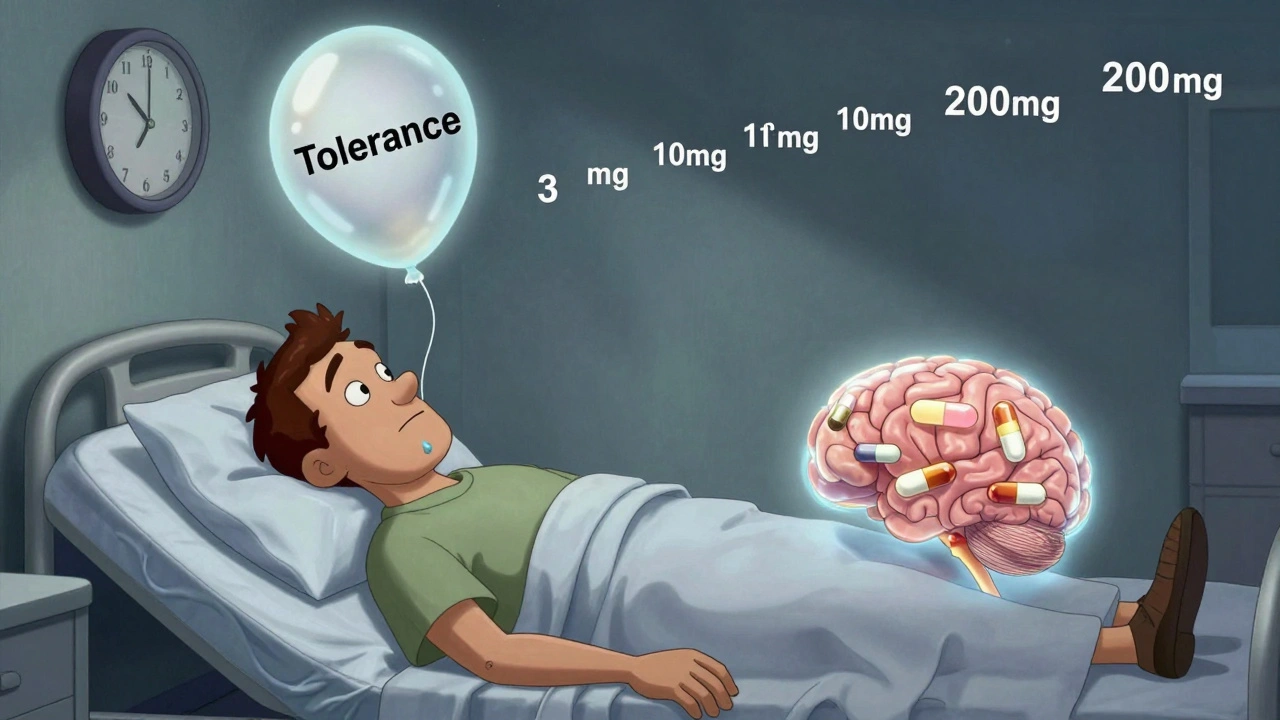
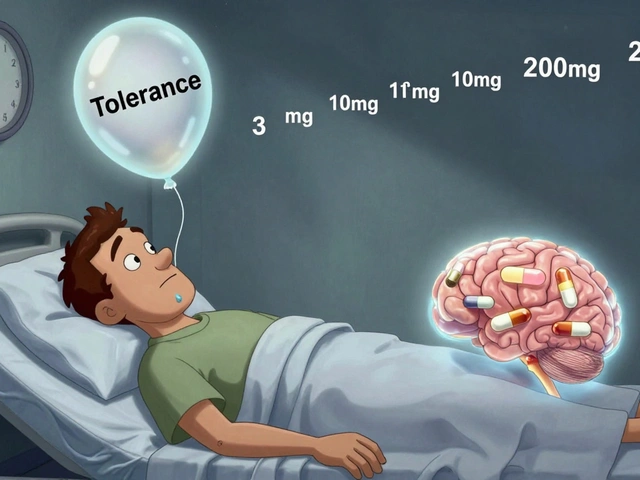
How Tolerance Builds-And Why It’s Dangerous
Tolerance isn’t just needing a higher dose. It’s your brain rewiring itself to ignore the drug’s effects. Every time opioids bind to mu-opioid receptors in your brain and spinal cord, they trigger dopamine release, reduce pain signals, and slow breathing. With repeated use, your body fights back. Receptors start to shrink in number. Cells become less responsive. Enzymes that break down the drug ramp up. This is called receptor downregulation and metabolic adaptation.
What’s scary is that tolerance doesn’t happen evenly. You might need twice as much to feel the same pain relief-but your body never fully adapts to the respiratory depression opioids cause. That’s the deadly gap. A person might be able to take 200 mg of oxycodone without feeling high, but that same dose can still shut down their breathing. The National Institute on Drug Abuse confirms that tolerance to euphoria develops faster than tolerance to respiratory suppression. That’s why even long-term users are at risk.
Studies show that within six months of daily opioid use, patients often need 25-50% higher doses just to manage pain. In one study, 32% of people prescribed opioids for chronic pain started misusing them within a year-not because they were seeking highs, but because the pain returned and their body needed more.
Dependence: When Stopping Feels Impossible
Dependence is different from addiction. You can be physically dependent without craving the drug or using it compulsively. It’s your body saying, ‘I need this to feel normal.’ When you stop, your nervous system goes into overdrive. Sweating, shaking, nausea, insomnia, muscle aches-these aren’t just discomforts. They’re signs your brain is struggling to restart its own pain and mood systems without opioids.
That’s why doctors don’t just stop someone’s prescription cold. Tapering slowly helps avoid withdrawal, but even then, the body remembers. Many people relapse not because they want to get high, but because the physical symptoms of withdrawal are unbearable. And here’s the cruel twist: the longer you’ve used, the longer withdrawal can last. Some report lingering anxiety, sleep issues, and pain sensitivity for months after quitting.
Dependence doesn’t mean you’re weak. It means your biology has changed. Even people who take opioids exactly as prescribed can become dependent. That’s why the CDC recommends limiting prescriptions to three days for acute pain and avoiding long-term use unless absolutely necessary.

Overdose: Why It Happens-Even to Experienced Users
An opioid overdose isn’t just taking too much. It’s your breathing slowing until it stops. Opioids suppress the brainstem’s drive to breathe. Normally, your body detects rising carbon dioxide and tells you to take a breath. Opioids silence that signal.
The biggest killer today isn’t prescription pills. It’s fentanyl. This synthetic opioid is 50 to 100 times stronger than morphine. Just 2 milligrams can kill. And it’s often mixed into other drugs-heroin, cocaine, counterfeit pills-without the user knowing. In 2021, synthetic opioids like fentanyl were involved in over 70% of all opioid overdose deaths in the U.S., up from just 20% in 2015.
But here’s what most people don’t realize: you don’t have to be a heavy user to overdose. People who’ve been clean for weeks or months are at the highest risk. Their tolerance drops fast. If they use their old dose, their body can’t handle it. A 2017 study found that 65% of opioid overdose deaths occurred in people who had previously been treated for addiction. One Reddit user wrote: ‘After 6 months clean, I used my old dose and nearly died-paramedics said I was clinically dead for 4 minutes.’
That’s why harm reduction programs push for naloxone (Narcan) access. Naloxone reverses opioid overdose by kicking the drug off the receptors. It’s safe, easy to use, and saves lives. Communities that distribute it widely have seen fatal overdoses drop by 34%.
The Safety Edge: Buprenorphine and Other Alternatives
Not all opioids are equally dangerous. Buprenorphine is a partial agonist. It activates opioid receptors-but only enough to ease withdrawal and cravings, without causing intense euphoria or full respiratory depression. It has a ceiling effect: after a certain dose, more doesn’t mean stronger high or greater risk. That’s why it’s used in Medication-Assisted Treatment (MAT).
Studies show MAT reduces overdose risk by 50%. In 2023, the U.S. passed the Mainstreaming Addiction Treatment (MAT) Act, allowing all licensed doctors-not just specialists-to prescribe buprenorphine. That’s a huge shift. Before, only 150,000 doctors could prescribe it. Now, over 1 million can.
Methadone also helps, but it’s riskier. It’s a full agonist with a long half-life, meaning it stays in the body for days. That makes it effective for maintenance but dangerous if misused or mixed with other depressants like alcohol or benzodiazepines.
Heroin users face another hidden danger: genetic differences in how their bodies metabolize it. Some people break down heroin faster, others slower. That’s why two people can take the same dose and have wildly different outcomes.

What’s Changing-And What Still Needs to Change
The opioid crisis isn’t static. Prescriptions have dropped sharply since 2012. In 2021, doctors wrote 46.7 prescriptions per 100 people-down from 81.3 in 2012. But illicit fentanyl has filled the gap. The DEA reports a 1,200% increase in fentanyl seizures between 2015 and 2022.
There’s progress. The FDA now requires opioid manufacturers to fund education on tolerance and overdose risk. New formulations like AVERSION technology make pills harder to crush or inject, though they don’t stop tolerance. The NIH has poured $1.5 billion into research for non-addictive pain treatments and better overdose reversal tools.
But the core problem remains: we still don’t have painkillers as powerful as opioids without their risks. Until then, the best defense is awareness. If you’re prescribed opioids, know your dose. Never mix them with alcohol or sleep aids. Keep naloxone on hand if you or someone you know uses opioids. And if you’ve quit-never use your old dose again. Your tolerance is gone. Your risk is higher than ever.
What to Do If You or Someone You Know Is Struggling
- If you’re on opioids for pain: Talk to your doctor about non-opioid options like physical therapy, NSAIDs, or nerve blocks. Ask if your dose is still necessary.
- If you’re trying to quit: Don’t go cold turkey. MAT with buprenorphine or methadone is safer and more effective. Call a local treatment center.
- If you’ve been clean: Never use your old dose. Your body has forgotten how to handle it. Start with a fraction. Have naloxone ready.
- If you see someone overdosing: Call 911. Give naloxone if you have it. Keep giving rescue breaths until help arrives. Naloxone wears off before opioids do-so you might need to re-dose.
There’s no shame in needing help. Opioids change your brain chemistry. That’s biology, not weakness. Recovery isn’t about willpower. It’s about access to care, support, and tools like naloxone and buprenorphine.
Can you become addicted to opioids if you take them as prescribed?
Yes. Addiction involves compulsive use despite harm, but dependence-your body needing the drug to function normally-can happen even with perfect use. Studies show up to 32% of patients on long-term opioid prescriptions develop misuse behaviors. That doesn’t mean everyone gets addicted, but the risk is real and often underestimated.
Why do people overdose after being clean for months?
Tolerance drops quickly after stopping opioid use. Your body no longer expects the drug, so your system can’t handle the same dose. Many overdose deaths happen in people who relapse after weeks or months of abstinence. They use their old dose-and their breathing stops because their tolerance is gone. This is why harm reduction programs stress never using your previous dose after a break.
Is fentanyl more dangerous than heroin?
Yes. Fentanyl is 50 to 100 times stronger than morphine and much more potent than heroin. It’s often mixed into other drugs without the user’s knowledge. A tiny amount-2 milligrams-can be lethal. In 2021, synthetic opioids like fentanyl caused over 70% of opioid overdose deaths in the U.S., up from 20% in 2015. Heroin is still dangerous, but fentanyl has become the primary driver of fatal overdoses.
Does naloxone work on all opioids?
Yes. Naloxone reverses the effects of all opioids-including morphine, oxycodone, heroin, and fentanyl-by blocking opioid receptors. It doesn’t work on other drugs like alcohol, cocaine, or benzodiazepines. But since most overdose deaths involve opioids, naloxone is the most effective first response. It’s safe, easy to use, and can be carried by anyone.
Can buprenorphine help with pain too?
Yes. Buprenorphine is used both for opioid use disorder and chronic pain. It’s less likely to cause respiratory depression than full agonists like oxycodone or fentanyl. But it’s not always the best choice for severe acute pain. Doctors weigh the benefits of pain relief against the risk of dependence. For many, it’s a bridge-reducing cravings while managing pain without the high risk of overdose.




Comments
Annie Gardiner
December 7, 2025
Okay but have you ever considered that tolerance isn't the problem-it's the fact that we treat pain like a bug to be erased, not a signal to be understood? My grandma had back pain for 40 years and never took opioids. She did yoga, ice packs, and refused to be a patient. We’ve medicalized suffering so hard we forgot how to just… sit with it.
Rashmi Gupta
December 8, 2025
India has 1.4 billion people. We have zero opioid crisis. Why? Because we don’t prescribe them like candy. We have turmeric, ayurveda, acupuncture, and a culture that says ‘wait, breathe, endure.’ Maybe the West needs less science and more silence.
Kumar Shubhranshu
December 9, 2025
Tolerance increases. Breathing suppression doesn’t. That’s the kill switch. End of story.
Mayur Panchamia
December 11, 2025
Oh great-another American sob story dressed up as science. We’re exporting this mess globally and now you want to lecture the world on ‘harm reduction’? We in India don’t need your naloxone. We need you to stop pushing pills like they’re Advil. Your healthcare system is a casino. Opioids are the house’s edge.
Kenny Pakade
December 11, 2025
Why are we even talking about this? It’s simple: if you’re dumb enough to get addicted to painkillers, you deserve what you get. Stop coddling junkies. Lock ‘em up. Or better yet-don’t prescribe them in the first place. End of debate.
Gwyneth Agnes
December 13, 2025
If you’re prescribed opioids, you’re already failing at life. Pain is a teacher. You’re just too weak to listen.
Ashish Vazirani
December 14, 2025
Let me tell you what REALLY happened in 2015-Big Pharma bought Congress, the FDA fell asleep, and doctors became drug reps with stethoscopes. Fentanyl? It’s not a drug-it’s a weapon. And someone’s making billions while kids die in alleyways. This isn’t science. This is genocide with a white coat.
Kay Jolie
December 14, 2025
It’s fascinating how the neuroplasticity of mu-opioid receptor downregulation intersects with the socio-psychoeconomic precarity of chronic pain management in late-stage capitalism-especially when you factor in the pharmacokinetic ceiling effect of partial agonists like buprenorphine as a structural intervention against allostatic overload. Naloxone isn’t just a reversal agent-it’s a symbolic rupture in the biopolitical control of bodily autonomy.
Max Manoles
December 14, 2025
I’ve been on buprenorphine for three years. It didn’t fix my pain. But it let me live again. I work. I hug my daughter. I sleep without nightmares. This isn’t about willpower. It’s about access. If your doctor won’t prescribe it, find another one. And if you’re reading this and scared-reach out. You’re not alone.
Arjun Deva
December 15, 2025
Wait-did you know the government puts fentanyl in street drugs on purpose to reduce the population? It’s in the CDC’s 2018 budget memo under ‘population control initiative.’ They don’t want old people living too long. And they’re using opioid deaths as cover. I saw the redacted page. Someone deleted the footnotes. Don’t trust the narrative.
Priya Ranjan
December 17, 2025
People who use opioids are lazy, entitled, and morally bankrupt. They choose drugs over discipline. If you can’t handle pain, you shouldn’t be allowed to drive, vote, or have kids. This isn’t a medical issue-it’s a character failure. And no, naloxone shouldn’t be free. Let them pay for their mistakes.
Write a comment