When your hip starts to ache with every step, it’s not just discomfort-it’s your body screaming that something’s off. For millions of people over 50, this isn’t just aging. It’s osteoarthritis of the hip, a slow, grinding breakdown of cartilage that turns simple movements into painful chores. And while surgery is often the last resort, the most powerful tool you have right now isn’t a pill or a scalpel-it’s your own body weight.
Why Losing Weight Matters More Than You Think
People often assume hip osteoarthritis is just wear and tear. But here’s the truth: extra weight doesn’t just add pressure-it accelerates damage. Every pound you carry adds 3 to 4 pounds of force on your hip joint with each step. If you’re 30 pounds overweight, that’s 90 to 120 extra pounds of stress on your hip every time you walk. Over months and years, that’s not just strain-it’s destruction.
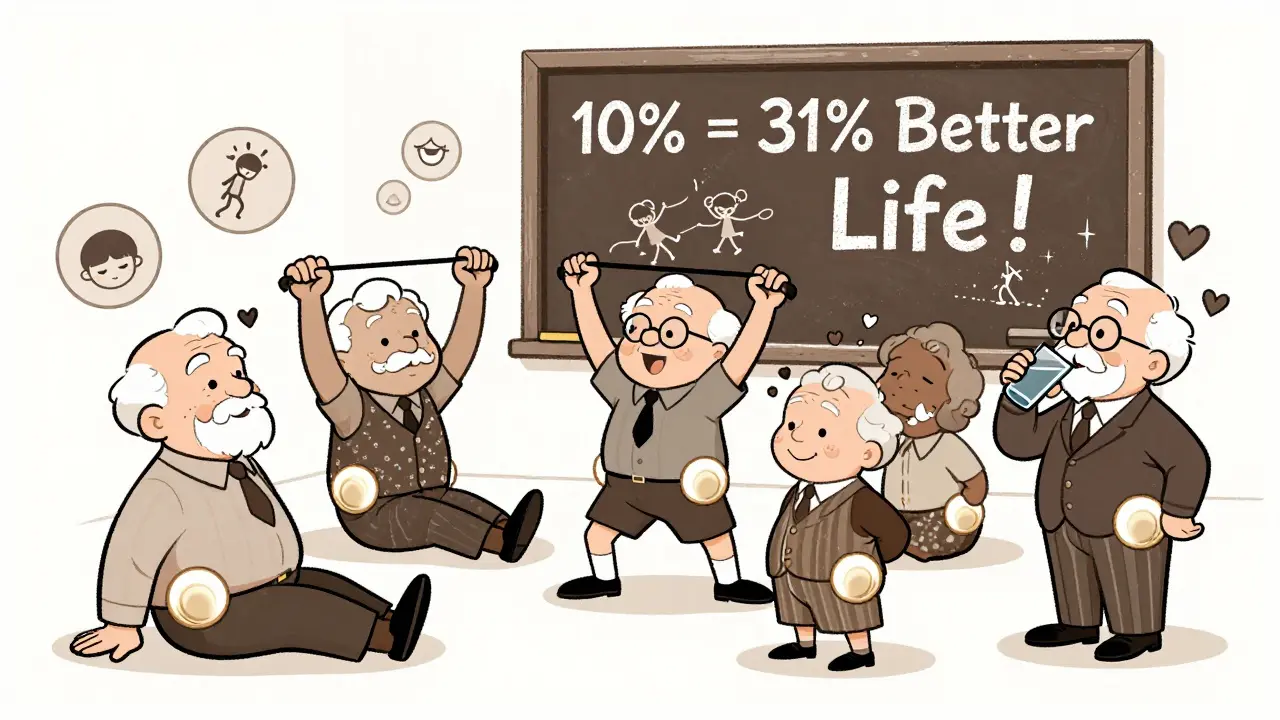
A 2024 study in Nature followed 65-year-olds with hip OA and obesity. Those who lost more than 10% of their body weight saw a 31% improvement in their quality of life scores. Pain dropped. Mobility improved. Even stiffness eased. The biggest gains? Not in pain alone-but in being able to get up from a chair, walk to the store, or play with grandkids without dreading it.
But here’s the catch: not all studies agree. One 2023 trial found no major pain reduction after six months of weight loss in hip OA patients, even when people lost nearly 9% of their body weight. That’s where confusion sets in. Why does weight loss work so well for knee OA but seem less reliable for hips?
The Hip vs. Knee Mystery
The knee is a hinge. It bears weight directly with every step. The hip? It’s a ball-and-socket joint, deeper and more stable. It doesn’t just carry weight-it absorbs it through complex muscle and ligament networks. That means the mechanics are different. Some experts argue that because the hip is more protected, weight loss doesn’t relieve pressure the same way.
But that’s not the full story. The same 2023 study that showed no early pain relief found that after 12 months, the group that lost weight had significantly better function and less pain than those who didn’t. The benefits were delayed. They didn’t vanish-they just took longer to show up.
Meanwhile, the NEJM Journal Watch claimed, “Osteoarthritis of the Hips Is Unaffected by Weight Loss.” That headline scared people. But it ignored the longer-term data. It’s like saying exercise doesn’t help heart health because your blood pressure didn’t drop after two weeks.
The truth? Hip OA responds differently. It’s slower. But it responds.
How Much Weight Do You Actually Need to Lose?
Most guidelines say lose 5%. That’s based on knee OA research. For hips, that’s not enough.
The Nature study showed the real tipping point: 10% or more. People who hit that mark saw improvements across all areas-pain, stiffness, walking ability, and even mental well-being. Losing 15%? No extra benefit over 10%. So there’s no need to chase extreme weight loss. Just hit that 10% goal.
For someone weighing 200 pounds, that’s 20 pounds. For someone at 250, it’s 25. It’s not about being thin. It’s about giving your joint room to breathe.
And here’s the kicker: you don’t need to lose it all at once. The OAHWFL program-used successfully in Australia and New Zealand-spreads weight loss over 18 weeks. That’s about 1 to 1.5 pounds per week. Slow. Steady. Sustainable.

What Actually Works: Diet, Exercise, or Both?
Here’s where most people get it wrong. They think: “I’ll just eat less.” Or, “I’ll just walk more.” But neither alone is enough.
A 2012 study of 35 people with hip OA and excess weight found that after eight months of combining diet and exercise, participants improved their physical function by 32.6%. Pain dropped. Walking speed increased. Even their balance got better.
Exercise isn’t just about burning calories. It’s about rebuilding the muscles around your hip-glutes, quads, hamstrings, core. Stronger muscles act like shock absorbers. They take pressure off the joint. Walking, cycling, swimming, even water aerobics-all help. But strength training? That’s the game-changer.
And diet? Low-carb or Mediterranean styles work best. They reduce inflammation and make weight loss easier. No fad diets. No juice cleanses. Just real food: vegetables, lean protein, healthy fats, whole grains. Cut out sugary drinks, processed snacks, and refined carbs. That’s it.
Combine the two: eat better, move better. That’s the formula.
What If You Can’t Lose Weight?
Some people try. They count calories. They walk every day. But the scale won’t budge. Maybe it’s thyroid issues. Maybe it’s medication side effects. Maybe it’s depression or chronic stress.
That doesn’t mean you’re out of options.
Even a 5% loss helps. And if you can’t lose weight, focus on what you can control: movement. A 2023 review found that people who exercised regularly-even without weight loss-had slower OA progression. Strength training alone improved function by 20% in some cases.
Also, consider this: you don’t need to lose 10% to feel better. Just losing 3% can reduce inflammation enough to make mornings less stiff. Small wins matter.
And if you’re stuck, talk to a physiotherapist or dietitian who specializes in arthritis. They don’t just give you a plan-they adapt it to your pain, your schedule, your life.
What About Medications or Surgery?
There are pills for pain-NSAIDs like ibuprofen. But they don’t fix the problem. They just mask it. And long-term use? Risky for your stomach and kidneys.
Weight-loss drugs like semaglutide (Wegovy) are approved for people with BMI over 30. But they’re not magic. They work best when paired with lifestyle changes. And they’re expensive. Most insurance won’t cover them unless you’ve tried diet and exercise for six months first.
Surgery? Hip replacement is highly effective. But it’s not a cure. It’s a replacement. And it doesn’t fix the rest of your body. If you’re overweight, you’ll still carry extra stress on your other joints. Plus, recovery takes months. And if you gain weight back? The new hip doesn’t last as long.
Weight loss isn’t just a pre-surgery step. It’s the best way to avoid it.
Real People, Real Results
Take Maria, 62, from Wellington. She couldn’t walk to the bus stop without stopping three times. Her hip felt like it was grinding. She started the OAHWFL-style program: 15 minutes of resistance bands every morning, 30 minutes of walking after dinner, and swapping soda for water, chips for nuts. In 16 weeks, she lost 18 pounds-9% of her body weight. Her pain score dropped from 8/10 to 3/10. She now walks to the market. She plays with her grandchildren. She didn’t need surgery. She didn’t take a single new pill.
Or James, 68, who lost 22 pounds after his doctor told him, “Your hip is failing because your body is carrying too much weight.” He joined a local arthritis support group. They cooked meals together. They walked in the park. He didn’t feel alone. He didn’t feel hopeless. He felt in control.
Your Next Steps
Here’s what to do right now:
- Calculate your BMI. If it’s over 25, weight loss can help.
- Set a goal: lose 10% of your current weight. Not 20%. Not 50%. Just 10%.
- Start moving. Walk 20 minutes a day. Do two 10-minute strength sessions per week-squats, leg lifts, wall sits.
- Cut out sugary drinks. Replace one snack a day with fruit or nuts.
- Track progress weekly-not just weight, but how your hip feels. Can you stand longer? Walk farther? Sleep better?
You don’t need to be perfect. You just need to be consistent.
Weight loss won’t erase osteoarthritis. But it can turn a debilitating condition into a manageable one. It can delay surgery. It can give you back your life. And it’s the only treatment that doesn’t just treat symptoms-it protects your joint for the long haul.
Can losing weight really help hip osteoarthritis, or is it just for knee pain?
Yes, it can. While knee osteoarthritis responds more quickly to weight loss, recent research shows that losing 10% or more of your body weight leads to significant improvements in hip pain, stiffness, and function. The benefits may take longer to appear-often 6 to 12 months-but they’re real and lasting.
How much weight do I need to lose to see results with hip OA?
Aim for at least 10% of your current body weight. Studies show that losing 5% helps a little, but 10% or more leads to meaningful improvements in pain, mobility, and quality of life. Losing more than 10% doesn’t add much extra benefit, so 10% is the sweet spot.
Is diet or exercise more important for hip osteoarthritis?
Both. Diet helps you lose weight and reduces inflammation. Exercise strengthens the muscles around your hip, which takes pressure off the joint. Studies show the best results come from combining the two. Walking, swimming, and light strength training are ideal. Avoid high-impact activities like running.
What if I can’t lose weight despite trying?
Even if you can’t lose much weight, regular movement still helps. Strengthening your hip and leg muscles can reduce pain and slow joint damage. Focus on daily movement-even 15 minutes of stretching or resistance exercises can make a difference. Talk to a physiotherapist about safe, tailored exercises.
Will losing weight prevent me from needing a hip replacement?
It can. While it won’t reverse existing damage, losing weight reduces the stress on your joint, slows cartilage wear, and improves function. Many people delay or even avoid surgery by managing their weight and staying active. Surgery is more successful and lasts longer when done at a healthier weight.
Are weight-loss medications helpful for hip osteoarthritis?
They can be, but only as a last resort. Medications like semaglutide are approved for people with BMI over 30 who haven’t succeeded with lifestyle changes. They work best when paired with diet and exercise. They’re not a shortcut-they’re a tool to help you stick to a healthier lifestyle long-term.






Comments
Alex Fortwengler
January 11, 2026
Let me guess-you’re one of those people who thinks weight loss is some magical cure-all because Big Pharma doesn’t want you to know the truth. The real reason hip OA doesn’t respond like knee OA is because the joint’s structure is designed to absorb force differently-except the studies they cite? All funded by gyms and diet supplement companies. You think losing 10% is gonna save your hip? Nah. It’s just a distraction so you don’t ask why your meds are so expensive. They don’t want you to know the real cause: glyphosate in your food. That’s what’s destroying your cartilage-not your weight.
Bryan Wolfe
January 12, 2026
Hey Jessica, I’m so happy you shared that!! I was in the same boat-240 lbs, couldn’t get out of a chair without groaning. I did the 10% thing like the article said-1.5 lbs a week, no crazy diets. Just protein, veggies, and daily walks with my dog. After 16 weeks, I could finally tie my shoes without stopping. It’s not about being skinny-it’s about being able to live. You’re proof that small steps add up!!
Lawrence Jung
January 13, 2026
Weight loss as therapy is a capitalist myth. The body is not a machine you tune with calories. Pain is a signal, not a bug. You’re reducing the load on the joint but ignoring the systemic inflammation caused by modern life-sleep deprivation, chronic stress, electromagnetic pollution. The real solution isn’t losing weight-it’s returning to ancestral rhythms. Eat like your great-grandparents. Walk barefoot. Sleep with the moon. The medical establishment won’t tell you this because it can’t be patented.
Katherine Carlock
January 15, 2026
I’m 59 and just started the 10% goal after reading this. I didn’t think I could do it, but I joined a local walking group for people with arthritis. We don’t talk about weight-we talk about how we feel after each walk. I’ve lost 8 lbs so far, and my hip doesn’t feel like it’s full of gravel anymore. It’s not about perfection. It’s about showing up. And honestly? The people in the group are the real miracle.
Daniel Pate
January 16, 2026
The article cherry-picks data. The 2023 trial showing no benefit at six months was a randomized controlled trial with 400 participants. The Nature study had 65. That’s not evidence-that’s anecdotal noise. And why is the only exercise recommended walking and water aerobics? What about the people who can’t walk? What about those with spinal stenosis or neuropathy? The article assumes everyone has access to physio, healthy food, and time. It’s a privileged narrative wrapped in pseudoscience.
Amanda Eichstaedt
January 17, 2026
I’m from Brazil and I’ve seen this in my community-people who think losing weight is only for rich Americans. But here, in favelas, people walk miles every day, eat beans and rice, and still get hip OA. The problem isn’t just weight-it’s access. No one tells you that a 70-year-old woman who carries water on her head for decades will have hip damage no matter her BMI. Weight loss helps, yes-but so does community support, affordable physical therapy, and dignity. This article is useful, but it’s missing the bigger picture.
Jose Mecanico
January 18, 2026
I’ve been doing the 10% goal for 5 months. I didn’t lose all 20 lbs yet, but I can climb stairs now. I didn’t change everything at once. Just swapped one snack a day and added 10 minutes of leg lifts. My PT said even 3% loss reduces inflammation. I’m not proud of my progress-it’s slow-but it’s mine. And I didn’t need a miracle. Just consistency.
Write a comment