When someone starts taking an antipsychotic medication, the goal is clear: reduce hallucinations, calm delusions, and bring back some stability. But for many, the relief comes with a hidden cost-rapid weight gain, rising blood sugar, and a spike in cholesterol. These aren’t just inconvenient side effects. They’re life-threatening risks that can shorten a person’s life by decades. The truth is, antipsychotic side effects involving metabolism are more dangerous than most patients and even some doctors realize.
Why Metabolic Risks Are a Silent Crisis
Second-generation antipsychotics (SGAs) like olanzapine, clozapine, and quetiapine were meant to be safer than older drugs. They were supposed to reduce tremors and muscle stiffness. And they did. But in the 2000s, a troubling pattern emerged: patients on these medications were gaining weight fast, developing type 2 diabetes, and showing signs of heart disease years before they should have. A 2023 review in Frontiers in Psychiatry found that people with serious mental illness live 20 to 25 years less than the general population-and about 60% of those early deaths come from heart disease and diabetes, not suicide or accident. The problem isn’t just lifestyle. Even people who eat well and exercise can see their blood sugar and cholesterol jump after starting an antipsychotic. That’s because these drugs interfere with how the body processes energy. They block receptors in the brain that control hunger and insulin, making it harder to feel full and easier for sugar to build up in the blood.Which Antipsychotics Carry the Highest Risk?
Not all antipsychotics are created equal when it comes to metabolic damage. The risk varies dramatically from one drug to another.- Olanzapine and clozapine are the worst offenders. In the CATIE study, patients gained an average of 2 pounds per month during the first 18 months. About 30% gained more than 7% of their body weight. Blood sugar levels rose sharply-even in people who didn’t gain much weight.
- Quetiapine and risperidone come next. Around 10-20% of users experience significant weight gain. Blood sugar and triglycerides tend to rise, but not as severely as with olanzapine.
- Aripiprazole, ziprasidone, and lurasidone are the safest options. Less than 5% of users gain more than 7% of their body weight. Blood sugar and cholesterol levels stay mostly stable.
What Exactly Happens in the Body?
It’s not just about eating more. Antipsychotics mess with your body’s internal systems in multiple ways:- Appetite control: They block H1 histamine receptors in the hypothalamus, the brain’s hunger center. This makes you feel hungry all the time, even after eating.
- Insulin resistance: Drugs like olanzapine interfere with how insulin works in muscle and fat cells. Sugar stays in the blood instead of being used for energy.
- Lipid metabolism: Triglycerides rise, HDL (good cholesterol) drops. This creates a perfect storm for plaque buildup in arteries.
- Fat storage: Fat cells become more efficient at storing energy, especially around the belly. Central obesity is one of the key signs of metabolic syndrome.
Metabolic Syndrome: The Silent Killer
Metabolic syndrome isn’t a single disease. It’s a cluster of conditions that together raise your risk of heart attack, stroke, and diabetes. The International Diabetes Federation defines it as:- Waist circumference: over 94 cm in men, 80 cm in women (ethnicity-adjusted)
- Plus any two of:
- Fasting blood glucose ≥100 mg/dL
- Triglycerides ≥150 mg/dL
- HDL cholesterol: below 40 mg/dL (men), below 50 mg/dL (women)
- Blood pressure ≥130/85 mmHg

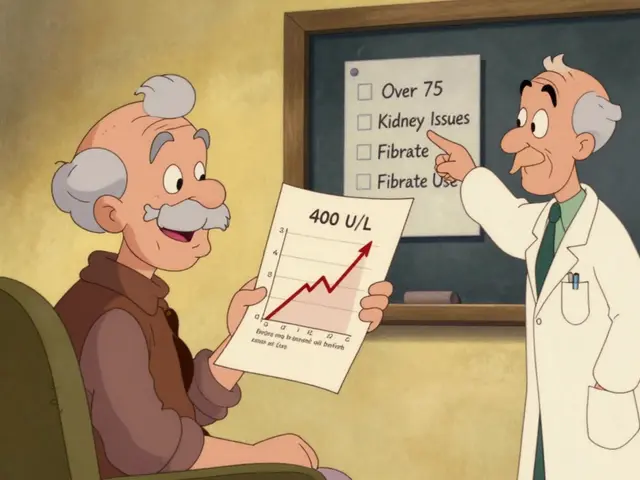
What Should Be Monitored-and When?
Guidelines from the American Psychiatric Association and the American Diabetes Association are clear: you can’t wait for symptoms to appear. You need to check before, during, and after starting treatment. Baseline (before starting):- Weight and BMI
- Waist circumference
- Blood pressure
- Fasting blood glucose
- Lipid panel (total cholesterol, triglycerides, HDL, LDL)
- At 4 weeks: weight, blood pressure
- At 12 weeks: full metabolic panel (glucose, lipids)
- At 6 months: repeat full panel
- Every year after: full panel, weight, waist, blood pressure
Why So Many Patients Are Falling Through the Cracks
You’d think this would be standard practice. But it’s not. A 2022 survey found that only 38% of U.S. psychiatrists consistently follow the recommended monitoring schedule. Why? Time. Lack of coordination. Poor record systems. Many patients see their psychiatrist every few months but never see a primary care doctor. No one checks their blood sugar. No one measures their waist. No one talks about diet or exercise. Patients themselves often don’t know what to ask. One Reddit user shared: “I gained 45 pounds in six months. My psychiatrist didn’t mention it. I only found out I had prediabetes when I went for a routine check-up with my GP.” Others feel trapped. “I stopped taking my meds because I gained 30kg in a year,” wrote a user on a UK mental health forum. “My doctor didn’t care about my blood sugar. I chose my mind over my body.” And then there are those who accept the trade-off. On PatientsLikeMe, 82% of clozapine users said the weight gain and high cholesterol were worth it because their psychosis was under control. That’s the cruel reality: sometimes the best treatment for the mind harms the body.What Works: Real Solutions That Help
It’s not all bleak. There are proven ways to reduce these risks. Medication switching: If someone gains weight fast on olanzapine, switching to aripiprazole or lurasidone can stabilize or even reverse metabolic damage. A 2023 study showed that patients who switched from olanzapine to lurasidone lost an average of 4.5 kg over 6 months. Lifestyle support: Just giving advice doesn’t work. But structured programs do. The Massachusetts General Hospital Freedom From Smoking program adapted its model for antipsychotic users and cut weight gain by half. They combined weekly nutrition coaching, group exercise, and medication reviews. Metformin: This diabetes drug is now commonly used off-label to prevent or treat antipsychotic-induced weight gain. Studies show it reduces weight gain by 3-5 kg over 6 months and improves insulin sensitivity. Integrated care: Kaiser Permanente started embedding dietitians and nurses in psychiatric clinics in 2019. Within two years, metabolic complications dropped by 25%. The key? Psychiatrists and primary care providers talking to each other.
What’s New in 2025?
The field is slowly changing. In 2023, the FDA approved lumateperone (Caplyta), a new antipsychotic with a much better metabolic profile. In clinical trials, only 3.5% of users gained significant weight-compared to 23.7% on olanzapine. The National Institute of Mental Health is funding a $12.5 million study to find genetic markers that predict who’s most likely to develop metabolic side effects. If successful, doctors could test a patient’s DNA before prescribing and choose the safest drug from the start. But progress is slow. Experts warn that if nothing changes, the life expectancy gap for people with serious mental illness could widen by another 5 years by 2030-mostly because of antipsychotic-related metabolic damage.What You Can Do
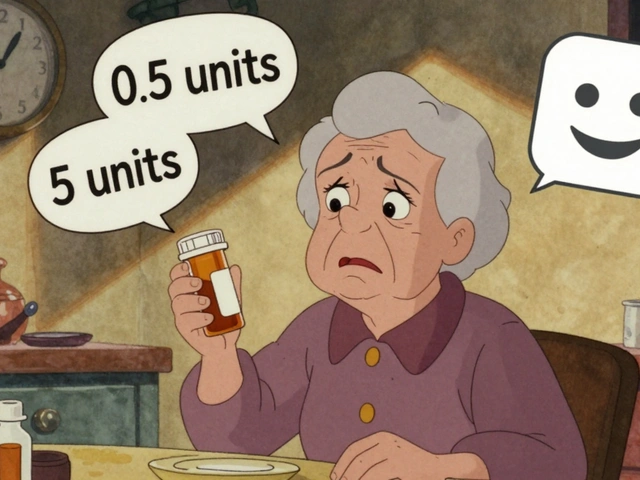
If you’re on an antipsychotic:- Ask your doctor for your baseline metabolic numbers before you start.
- Get your weight, waist, blood pressure, glucose, and lipids checked every 3 months for the first year.
- If you gain more than 5% of your body weight, don’t wait. Talk about switching meds or adding metformin.
- Request a referral to a dietitian or exercise program. Don’t assume you’re on your own.
- Keep a log of your weight and how you feel. Bring it to appointments.
- Don’t assume your patient knows the risks. Explain them plainly: “This drug can make you gain weight and raise your blood sugar. We’ll check it regularly.”
- Use a checklist. Put metabolic monitoring in your EHR as a mandatory step.
- Collaborate with primary care. Share records. Schedule joint visits if needed.
- Know your options. Aripiprazole and lurasidone aren’t just “alternatives”-they’re safer choices for many patients.
It’s Not a Trade-Off You Should Have to Make
No one should have to choose between mental stability and physical health. But right now, too many do. The tools to prevent this are already here: better drugs, proven monitoring, lifestyle support, and coordinated care. What’s missing is the will to use them. The goal isn’t just to treat psychosis. It’s to help people live longer, healthier lives. That means treating the whole person-not just the mind.Which antipsychotics cause the most weight gain?
Olanzapine and clozapine cause the most significant weight gain, with patients often gaining 2 pounds per month in the first 18 months. About 30% of users gain more than 7% of their body weight. Risperidone and quetiapine carry moderate risk, while aripiprazole, ziprasidone, and lurasidone have the lowest risk-often causing less than 5% weight gain.
How often should metabolic tests be done on antipsychotic patients?
Baseline tests (weight, waist, blood pressure, fasting glucose, lipids) should be done before starting treatment. Repeat checks at 4 weeks, 12 weeks, and then every 6 months for the first year. After that, annual monitoring is recommended. More frequent checks are needed if weight gain exceeds 5% or blood sugar/lipids rise.
Can antipsychotic-induced diabetes be reversed?
Yes, in many cases. Switching to a lower-risk antipsychotic like aripiprazole or lurasidone, combined with lifestyle changes and metformin, can improve insulin sensitivity and lower blood sugar. Some patients see their prediabetes reverse within 6-12 months. However, long-standing type 2 diabetes may require ongoing management.
Is metformin safe to take with antipsychotics?
Yes. Metformin is commonly prescribed off-label to counteract weight gain and insulin resistance caused by antipsychotics. Studies show it reduces weight gain by 3-5 kg over 6 months and improves metabolic markers without interfering with psychiatric treatment. Side effects like mild nausea or diarrhea usually improve after a few weeks.
Why don’t psychiatrists monitor metabolic health more often?
Many psychiatrists lack time, training, or access to lab services. Some assume patients will be monitored by primary care, but coordination is often poor. Others don’t realize how quickly metabolic damage can occur. Only 38% of U.S. psychiatrists consistently follow national monitoring guidelines, according to a 2022 survey.
Are there new antipsychotics with fewer side effects?
Yes. Lumateperone (Caplyta), approved by the FDA in 2023, has a significantly better metabolic profile. In trials, only 3.5% of users gained significant weight compared to 23.7% on olanzapine. Research is also underway to identify genetic markers that predict who’s at highest risk, paving the way for personalized prescribing.




Comments
Charles Barry
December 21, 2025
Let me guess-Big Pharma paid the FDA to approve these metabolic time bombs. Olanzapine? That’s not medicine, it’s a slow-acting poison disguised as a ‘stability drug.’ They don’t care if you die of diabetes in 10 years as long as you’re quiet and compliant. Wake up. The system is designed to chemically sedate the poor while the doctors collect their kickbacks. #PharmaLies
Rosemary O'Shea
December 22, 2025
Oh, how *quaint*. You’ve written a 2000-word manifesto on metabolic syndrome as if it were a novel discovery. The truth? We’ve known since the late 90s that SGAs wreak havoc on insulin signaling. What’s astonishing is how little has changed-because psychiatrists still treat the brain like a separate organ, not part of a biological ecosystem. The real scandal isn’t the side effects-it’s the institutional arrogance that refuses to integrate endocrinology into psychiatric care. Sigh.
Candy Cotton
December 22, 2025
As an American, I find it appalling that our healthcare system allows this to continue. We have the technology, the data, and the guidelines-but no political will. The fact that only 38% of psychiatrists follow monitoring protocols is a national disgrace. This isn’t just medical negligence-it’s a failure of American leadership in mental health. We must demand accountability, not just sympathy.
Jeremy Hendriks
December 22, 2025
Here’s the uncomfortable truth: we’ve turned psychiatric care into a chemical containment protocol. We don’t treat people-we manage symptoms with blunt instruments. The body isn’t a machine to be tweaked with drugs; it’s a dynamic, evolving organism. When you block H1 receptors to silence voices, you’re not curing psychosis-you’re silencing a cry for help with a pharmacological sledgehammer. The metabolic collapse? That’s the body screaming back. We’ve forgotten that healing requires harmony, not domination.
Tarun Sharma
December 24, 2025
Thank you for this comprehensive overview. The data is clear, and the recommendations are well-structured. In India, access to regular metabolic monitoring remains a challenge, especially in rural areas. However, the principles outlined here are universally applicable. Early intervention and patient education are critical. We must prioritize integrated care models, even with limited resources.
Gabriella da Silva Mendes
December 26, 2025
Ugh. I just got off olanzapine after gaining 50 lbs in 8 months. My psychiatrist said "it's normal" and handed me a pamphlet on "healthy eating." 😒 I’m not lazy-I’m medicated into a food coma. Metformin helped a little, but I still look like a balloon animal. Why is it that when your mind is broken, your body becomes a trash can? 🤡 I’m switching to aripiprazole next week. Pray for me.
Jim Brown
December 26, 2025
There is a profound metaphysical irony here: the very agents meant to restore mental clarity are systematically dismantling the physiological foundation of life itself. We have engineered a civilization that can map the human genome but cannot reconcile the mind’s need for peace with the body’s need for balance. Is this healing-or is it a quiet surrender to the myth that the soul can be saved while the flesh is sacrificed? The answer lies not in pharmacology, but in the courage to reimagine care as wholeness.
Sam Black
December 27, 2025
I’ve been on lurasidone for two years now-no weight gain, stable glucose, and my psychosis? Totally under control. It’s not a miracle drug, but it’s the closest thing we have to a responsible option. What helped me most was finding a dietitian who understood mental illness. She didn’t judge me for my cravings-she helped me work with them. If you’re struggling, don’t suffer in silence. Ask for help. There are people who get it.
Tony Du bled
December 29, 2025
Yeah, I’ve been on risperidone for 5 years. Gained 30 lbs. Got prediabetes. My doc never mentioned it until I brought it up. Then he shrugged and said, "Well, you’re not dead yet." So I’m switching to aripiprazole next month. Hope it works. If not, I’m done with meds. My mind’s better than my body right now.
Art Van Gelder
December 30, 2025
Let’s talk about the elephant in the room: we’re not just treating psychosis-we’re treating poverty, trauma, and systemic neglect with pills. The metabolic damage? It’s not just a side effect. It’s a symptom of a broken system. People on these meds are often homeless, uninsured, or stuck in underfunded clinics. Of course their blood sugar spikes-they’re eating processed food because it’s cheap, and they’re not getting exercise because they’re exhausted from surviving. We need more than monitoring protocols-we need housing, food access, and trauma-informed care. Otherwise, we’re just putting bandages on a hemorrhage.
Vikrant Sura
December 31, 2025
This post is just rehashing what’s been known for 15 years. No new data. No original insight. Just a long list of facts dressed up like a revelation. The real issue? Most patients don’t care. They’d rather be stable and obese than thin and hallucinating. Stop pretending this is a medical crisis-it’s a human one.
Write a comment