What Is Ascites, and Why Does It Happen?
Ascites isn’t just bloating. It’s fluid building up in your belly because your liver isn’t working right. This happens mostly in people with cirrhosis-when scar tissue replaces healthy liver tissue. About half of all cirrhosis patients will develop ascites within 10 years. Once it shows up, your risk of serious complications goes up. Half of these patients won’t survive past two years without proper management.
The root cause? High pressure in the veins around your liver (portal hypertension) and your kidneys holding onto too much salt and water. Your body thinks it’s low on blood volume, so it turns on survival mode: keep sodium, keep fluid. The result? Your belly swells. Your legs puff up. You feel full all the time-even when you haven’t eaten much.
Sodium Restriction: The Old Rule and the New Debate
For decades, the rule has been simple: eat less than 2 grams of sodium a day. That’s about 5 grams of salt-less than one teaspoon. Major guidelines from the American Association for the Study of Liver Diseases (AASLD) and others have pushed this hard. But here’s the problem: most people can’t stick to it.
Studies show fewer than 40% of patients actually follow strict sodium limits. Why? Because 75% of the sodium we eat comes from packaged foods, restaurant meals, and processed snacks-not the salt shaker. Trying to cut it all out feels impossible.
And now, new research is turning the old advice on its head. Two large studies published between 2017 and 2022 found that patients who ate 5-6.5 grams of salt per day (about 2-2.5 grams of sodium) had better results than those on the strict 2-gram plan. Their ascites cleared faster. They needed fewer fluid drains. And crucially, they were less likely to develop kidney problems.
Why would more salt help? Because going too low can hurt your kidneys. When sodium drops too far, blood flow to your kidneys slows down. That can trigger something called hepatorenal syndrome-a dangerous drop in kidney function that’s deadly in up to 35% of cases when sodium is overly restricted.
So what’s the real target now? Experts are shifting toward moderation. A 2023 review in Gut and Liver Journal concluded: “Sodium should not be restricted strictly in the treatment of cirrhotic ascites, particularly when patients are treated with diuretics.” Many hepatologists now aim for 3-4 grams of sodium daily-enough to avoid harm, but not so little that it backfires.
Diuretics: The Medication That Actually Moves the Fluid
Sodium restriction alone won’t fix ascites. You need diuretics-meds that make your kidneys flush out salt and water. The two main ones are spironolactone and furosemide.
Spironolactone is usually the first choice. It starts at 100 mg a day and can be slowly increased to 400 mg if needed. It works by blocking aldosterone, a hormone that makes your body hold onto salt. It’s slow but steady. You won’t see big changes in the first few days, but over time, the fluid drains.
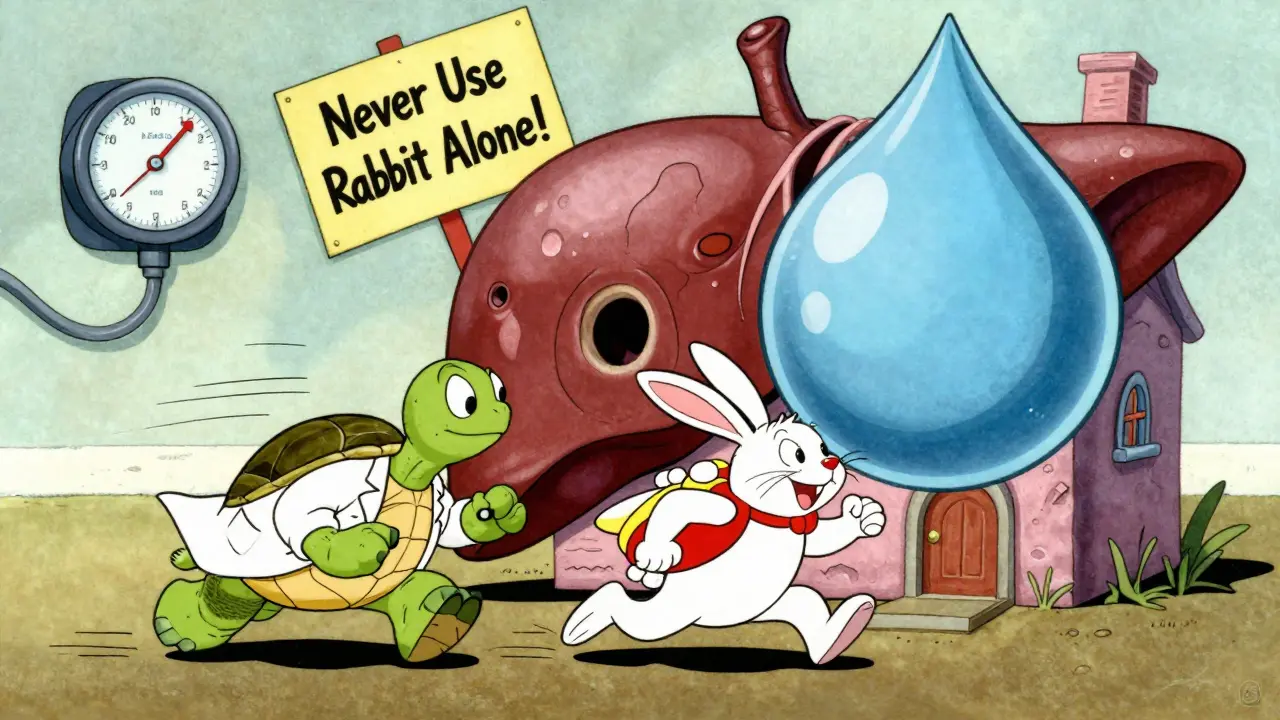
Furosemide is faster. It’s often added when spironolactone isn’t enough. Start at 40 mg daily, and you can go up to 160 mg if needed. But never use furosemide alone-it can crash your sodium levels and hurt your kidneys. Always combine it with spironolactone in a 1:2 or 1:3 ratio (like 100 mg spironolactone to 40 mg furosemide).
The goal? Lose no more than 0.5 kg (1 pound) per day if you don’t have swollen legs, or up to 1 kg (2 pounds) if you do. Go faster than that, and you risk low blood pressure, kidney failure, or dangerous electrolyte shifts.
Monitoring is critical. Your doctor will check your blood sodium at least twice a week when you start. If your sodium drops below 130, that’s a red flag. Too low, and you can get confused, dizzy, or even have seizures. That’s hyponatremia-and it’s common in ascites patients. If it happens, your diuretics may need to be lowered, or you might need IV fluids.
What Medications to Avoid
Some common drugs can make ascites worse-or even kill you. Avoid NSAIDs like ibuprofen or naproxen. They reduce blood flow to your kidneys, which can trigger kidney failure in cirrhosis patients.
ACE inhibitors and ARBs (blood pressure meds like lisinopril or losartan) are also risky. Studies show they raise the chance of end-stage kidney disease by 2.3 times in people with liver cirrhosis. If you’re on these for high blood pressure, talk to your doctor about switching to safer options like beta-blockers.
Even over-the-counter supplements can be dangerous. Herbal remedies like licorice root or certain weight-loss teas can interfere with sodium balance or damage your liver further. Always check with your hepatologist before taking anything new.
What If Diuretics Don’t Work?
For 5-10% of patients, ascites doesn’t respond to maximum doses of diuretics. That’s called refractory ascites. It’s serious. Survival drops to about 50% within six months without other treatment.
The go-to solution? Large-volume paracentesis. This is when a doctor inserts a needle into your belly and drains off 4-10 liters of fluid in one session. It’s quick, effective, and can be done as an outpatient. But here’s the catch: you must get albumin (a blood protein) given through an IV right after. For every liter of fluid removed, you need 8 grams of albumin. Skip this, and your blood pressure can crash.
Albumin replacement cuts complications from 15% down to under 5%. It’s expensive, but it saves lives.
Other options like vaptans (drugs that block water retention) are rarely used. They cost $5,000-$7,000 per course and are only approved for 30 days. They’re not better than paracentesis-and they don’t work for most people.

The Real Challenge: Living With It
Managing ascites isn’t just about pills and diet. It’s about daily choices. You can’t eat canned soup, deli meats, soy sauce, or frozen meals. You’ll need to cook from scratch-plain chicken, rice, fresh veggies, olive oil. That’s hard. It’s expensive. And it’s lonely.
Malnutrition is a silent killer here. Up to 90% of cirrhosis patients don’t get enough protein. Your body needs it to make albumin, which helps keep fluid from leaking into your belly. Eat protein at every meal: eggs, fish, lean meat, lentils. If you can’t eat enough, talk to your doctor about oral supplements.
And don’t ignore your mental health. Ascites makes you feel trapped in your own body. Depression and anxiety are common. Support groups, counseling, or even just talking to someone who’s been through it can make a huge difference.
What’s Next? The Big Study Coming in 2025
The debate over sodium isn’t settled. That’s why the PROMETHEUS trial (NCT04567890) is so important. It’s a major randomized study comparing a strict low-sodium diet (under 2 g/day) with a moderate one (5-6.5 g/day) in people with ascites. Results are expected by late 2025.
If the moderate group does better, guidelines will change. Doctors will stop pushing impossible restrictions. Patients will get better outcomes without feeling punished.
Until then, the best approach is personalized. If you’re on diuretics, eating 3-4 grams of sodium a day is likely safe-and maybe even better than going lower. Work with your care team. Track your weight daily. Watch for swelling. Report any confusion or dizziness. And don’t be afraid to ask: “Is this really helping me-or just following an old rule?”
Key Takeaways
- Ascites is a sign your liver disease is getting worse-and needs active treatment.
- Strict sodium restriction (under 2 g/day) is outdated for most people. Aim for 3-4 grams instead.
- Spironolactone and furosemide together are the standard treatment. Never use furosemide alone.
- Weight loss should be slow: no more than 0.5-1 kg per day.
- Avoid NSAIDs, ACE inhibitors, and ARBs-they can damage your kidneys.
- If diuretics don’t work, large-volume paracentesis with albumin is the next step.
- Protein intake is just as important as salt control. Don’t let malnutrition sneak up on you.




Comments
Kimberly Reker
January 29, 2026
Wow, this is one of the clearest breakdowns of ascites management I’ve ever read. I’ve been watching my dad go through this, and the sodium thing always confused me-everyone says ‘no salt!’ but then you realize half your food is secretly loaded with it. The part about 3-4g being safer than 2g? That’s a game-changer. I’m printing this out for his hepatologist.
Mike Rose
January 29, 2026
so like… we just eat more salt now? lol. i thought the whole point was to not swell up. this sounds like a scam to make me eat more chips.
Russ Kelemen
January 31, 2026
There’s something deeply human here-how medicine keeps trying to simplify complex biology into rigid rules, and then the body fights back. We’re not machines. Our kidneys aren’t programmable thermostats. The shift from ‘zero sodium’ to ‘moderate’ isn’t just clinical-it’s ethical. It’s about respecting the patient’s ability to live, not just survive. This isn’t permission to binge salt. It’s permission to breathe again.
Diksha Srivastava
February 1, 2026
This gives me so much hope! My uncle was told he had to eat only boiled rice and water for months… he lost weight, lost spirit, and still had the swelling. If 3-4g sodium is okay, maybe he could’ve had some dal and tomato curry. Food shouldn’t feel like punishment. Thank you for sharing this!
Sidhanth SY
February 2, 2026
Actually, the sodium debate makes sense when you think about it. If your body thinks it’s drowning in fluid but starving for salt, forcing it into starvation mode just makes it panic. It’s like trying to put out a fire by turning off the water supply. The diuretics are the hose, sodium is the fuel-too little and the engine stalls. 3-4g feels like the sweet spot.
Adarsh Uttral
February 3, 2026
bro i had ascites last year and they had me on spironolactone and furosemide. i thought i was doing good til i lost 3lbs in 2 days and nearly passed out. they told me to slow down but never said why. this post explains everything. thanks.
Write a comment