Medication Swelling Risk Checker
Swelling in your hands or feet might seem like a minor annoyance-maybe you wore tight shoes, stood too long, or ate something salty. But if it started after you began a new medication, it could be a sign your body is reacting in a way that needs attention. Medication-induced swelling isn’t always harmless. In fact, it’s one of the most common reasons people stop taking important drugs like blood pressure medications or cancer treatments.
What’s Actually Happening in Your Body?
Not all swelling is the same. There are two main types you need to know about. The first is vasodilator-induced edema. This happens when certain drugs, like calcium channel blockers (amlodipine, nifedipine), dilate your blood vessels. That sounds good for lowering blood pressure, but it also lets fluid leak out into your tissues, especially around your ankles and feet. You’ll notice pitting edema-press your skin and it holds a dent for a few seconds. This usually affects both legs equally, gets worse by evening, and improves after lying down overnight. The second type is hand-foot syndrome (also called palmar-plantar erythrodysesthesia). This one hits your palms and soles. It starts with redness, tingling, or numbness. Then comes swelling, peeling skin, and sometimes painful blisters. This is most common with chemotherapy drugs like capecitabine, where up to 60% of patients experience it. Unlike regular edema, this isn’t just fluid-it’s inflammation in the skin itself.Which Medications Are Most Likely to Cause Swelling?
Some drugs carry a much higher risk than others. Here’s what the data shows:- Calcium channel blockers (amlodipine, nifedipine): Up to 15% of people on standard doses develop ankle swelling. Dose matters-10mg amlodipine causes swelling in nearly 15% of users, while 5mg only affects about 4%.
- NSAIDs (ibuprofen, naproxen): Long-term use leads to noticeable swelling in 1-3% of users, mostly due to kidney effects that make your body hold onto sodium.
- Corticosteroids (prednisone): These cause fluid retention, often leading to puffiness in hands and feet.
- Thiazolidinediones (pioglitazone, rosiglitazone): Used for type 2 diabetes, they cause swelling in 4-7% of users within just three months.
- Chemotherapy agents (capecitabine, doxorubicin): Hand-foot syndrome affects up to 60% of patients on these drugs, especially with repeated cycles.
- Gabapentin and pregabalin: These nerve pain meds cause swelling in a significant number of users, often described as “sock marks that last all day.”
It’s not just the drug itself-it’s how it interacts with your body. Someone on multiple medications might have swelling from a combination, not just one. And if you’re older, have heart or kidney issues, or are inactive, your risk goes up.
When Is Swelling a Red Flag?
Not every bit of swelling needs an emergency room visit. But some signs mean you should call your doctor today:- One-sided swelling (only one foot or hand): Could be a blood clot (deep vein thrombosis). Left untreated, it can travel to your lungs.
- Swelling with chest pain, shortness of breath, or dizziness: These point to heart failure. Fluid backs up because your heart can’t pump properly.
- Rapid weight gain-more than 2 pounds in 24 hours or 5 pounds in a week: This is fluid overload, a sign your body is struggling to manage fluids.
- Blistering, open sores, or skin turning dark or purple: Especially with hand-foot syndrome. This is Grade 3 or higher, and it can become life-threatening.
- Swelling with little or no urine output (less than 500 mL per day): Your kidneys may be failing to filter fluids.
- Swelling that started within 72 hours of starting a new drug: There’s a 78% chance it’s drug-related, according to NIH data.
These aren’t “wait and see” situations. Delaying care increases the risk of serious complications. A 2023 FDA analysis found that 37% of severe outcomes from medication swelling happened because people waited too long-on average, 8.2 days after symptoms began.

What Should You Do If You Notice Swelling?
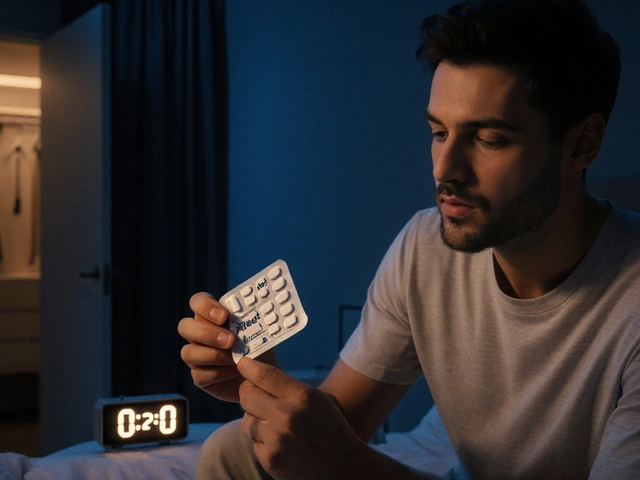
First, don’t panic. But don’t ignore it either. Here’s what to do next:- Check your meds. Look at what you started in the last 1-2 weeks. Write them down.
- Track the swelling. Is it only in your feet? Both hands and feet? Does it leave a dent? Is it getting worse?
- Take your weight daily. Use the same scale, same time of day (morning, before eating). A 2-pound jump in 24 hours is a red flag.
- Call your doctor. Don’t wait for your next appointment. Say: “I started [medication] and now my feet/hands are swollen. I’m concerned.”
Your doctor may:
- Lower your dose (especially for calcium channel blockers-switching from 10mg to 5mg amlodipine cuts swelling risk by more than half).
- Switch you to another drug (e.g., from amlodipine to losartan-studies show 85% of swelling resolves within two weeks).
- Add a low-dose ACE inhibitor to help reduce fluid buildup (60-70% effective).
- For hand-foot syndrome: reduce chemotherapy dose, apply cooling packs, or recommend special creams (though evidence is mixed).
What You Can Do at Home
While you wait to see your doctor-or as part of your treatment plan-these steps help:- Elevate your feet above heart level for 30 minutes, three times a day. This can reduce swelling by 15% in just 48 hours.
- Reduce sodium. Aim for under 2,300 mg per day. Skip processed foods, canned soups, and salty snacks.
- Wear compression stockings (20-30 mmHg pressure). Studies show they reduce swelling severity by 40%.
- Choose supportive shoes. Get ones with extra depth-your feet may swell up during the day.
- Moving matters. Walk regularly. Don’t sit or stand still for hours. Gentle movement helps fluid circulate.
- Time your diuretics. If you’re on a water pill, take it in the morning so you’re not waking up at night to pee.
Some people try vitamin B6 or arnica gel for hand-foot syndrome. But research is mixed. A 2022 Cochrane review found B6 didn’t help significantly. Arnica gel showed promise in one small study, but it’s not standard advice yet.

Why People Wait Too Long
A 2023 survey of 872 patients found that 55% didn’t call their doctor right away because they thought swelling was “normal” or “not serious.” That’s dangerous. Many assume it’s just aging, standing too long, or weight gain. But if it’s drug-related, it can get worse fast.On patient forums, people share stories like: “I couldn’t hold a toothbrush,” or “My socks left deep marks all day.” One user switched from amlodipine to losartan and had full swelling relief in five days. Another had to stop chemotherapy because hand-foot syndrome made it impossible to walk.
Early action makes all the difference. Studies show 89% of medication-induced swelling resolves within four weeks of proper intervention. But 11% turn into chronic lymphedema-lasting, hard-to-treat swelling that needs lifelong management.
Prevention Is Possible
You don’t have to wait for swelling to start. If you’re starting a high-risk medication:- Ask your doctor to start at the lowest effective dose. For amlodipine, that’s 2.5-5mg instead of 10mg.
- For chemotherapy: Some cancer centers recommend applying urea 10% cream to hands and feet twice daily. One trial showed a 25% drop in hand-foot syndrome incidence.
- Get educated. Patients who received clear instructions on what swelling looks like were 3.2 times more likely to seek help early.
There’s no guarantee you’ll avoid swelling, but knowing the signs and acting fast gives you control.
Can over-the-counter diuretics help with medication-induced swelling?
No. Over-the-counter diuretics (like caffeine pills or herbal supplements) aren’t safe or effective for this. They can worsen electrolyte imbalances, especially if you’re already on blood pressure or heart meds. Only use prescription diuretics under a doctor’s supervision.
Will the swelling go away if I stop the medication?
Usually, yes-but only if you stop under medical guidance. For calcium channel blockers, swelling often fades within 1-2 weeks after switching or lowering the dose. For chemotherapy-related hand-foot syndrome, symptoms improve after dose reduction or a treatment break. Never stop a medication on your own, especially if it’s for heart disease, diabetes, or cancer.
Is hand-foot syndrome the same as athlete’s foot?
No. Athlete’s foot is a fungal infection that causes itching, peeling, and redness between the toes. Hand-foot syndrome is caused by drugs, starts with tingling or burning, leads to redness and swelling on palms and soles, and can develop blisters or ulcers. It doesn’t spread like an infection and doesn’t respond to antifungal creams.
Can stress or diet cause this kind of swelling?
Stress and salty food can make swelling worse, but they don’t cause medication-induced edema on their own. If you’re on a drug known to cause swelling, those factors can amplify it. But if you didn’t start a new medication, the swelling likely has another cause-like heart, kidney, or liver issues.
How long does it take for swelling to go away after switching meds?
For calcium channel blocker swelling, most people see improvement within 7-14 days after switching to a different class of blood pressure drug, like an ACE inhibitor or ARB. For hand-foot syndrome, symptoms often begin to ease within 3-5 days after reducing the chemotherapy dose. Full resolution can take up to 4 weeks.





Comments
Tejas Bubane
December 8, 2025
Look, I've been on amlodipine for 3 years and my ankles look like overinflated balloons by 6pm. I didn't think it was the drug until I read this. Switched to losartan last month. Swelling cut in half in 10 days. No more sock marks. Why do doctors not tell you this upfront?
Lisa Whitesel
December 9, 2025
Stop taking drugs and your body won't swell
Larry Lieberman
December 10, 2025
Hand-foot syndrome is the worst 😩 I was on capecitabine and my palms felt like they were on fire. Took a break, used urea cream, and it calmed down. But man, the peeling... like I'd been sanding my hands with 80 grit. Don't ignore it. Your skin isn't just being dramatic.
Simran Chettiar
December 12, 2025
It is not merely the pharmacological agent that induces edema, but rather the systemic imbalance precipitated by its introduction into the homeostatic architecture of the human organism. One must consider the ontological weight of pharmaceutical intervention upon the corporeal vessel, especially when the vessel is already burdened by age, inactivity, or latent renal compromise. The body does not merely retain fluid-it resists the imposition of chemical hegemony.
Therefore, the question is not whether the drug causes swelling, but whether we have the moral fortitude to question why we subject ourselves to such interventions in the first place. Is comfort worth the slow erosion of bodily autonomy?
I have observed patients who, upon being prescribed pioglitazone, experience swelling within weeks. Yet they continue, fearing the consequences of non-adherence. This is not compliance-it is capitulation to a medical-industrial complex that profits from chronicity.
Perhaps we should begin with diet, movement, and mindfulness before reaching for the pill bottle. But no, the system demands pills. And so we swell.
And yet, I am not against medication. I am against the silence that surrounds its side effects. This post is a rare act of lucidity in a sea of pharmaceutical propaganda.
Anna Roh
December 14, 2025
My mom took prednisone for her arthritis and her face looked like a balloon. She didn't say anything for weeks. Then she couldn't zip her pants. Duh.
Philippa Barraclough
December 15, 2025
I appreciate the thorough breakdown of medication-induced edema types. The distinction between vasodilator-induced and hand-foot syndrome is critical, and too often conflated. I've seen patients in my clinic misdiagnose the latter as dermatitis or fungal infection, leading to inappropriate antifungal regimens and delayed dose adjustments. The NIH data on 78% likelihood of drug causation within 72 hours is particularly compelling. I would add that monitoring daily weights is underutilized in primary care. It's a simple, low-cost metric that can prevent hospitalizations. Also, compression stockings-while effective-are often dismissed as 'not glamorous.' Patients need to hear that their comfort matters as much as their lab values.
One point I'd clarify: the recommendation for ACE inhibitors to reduce swelling is context-dependent. In patients with renal artery stenosis or hyperkalemia, adding an ACEi could be dangerous. It's not a universal fix. Tailoring the response to comorbidities is essential.
And while vitamin B6 has been largely debunked, some anecdotal reports suggest topical menthol or aloe vera may offer symptomatic relief for hand-foot syndrome, even if not evidence-based. Sometimes, palliation is the goal when dose reduction isn't feasible.
Tiffany Sowby
December 16, 2025
Why are we even taking these drugs? In America, we're medicated to the point of collapse. My cousin had to stop chemo because her feet were bleeding. She didn't even get a warning. This is what happens when profit drives medicine, not care. You're supposed to just 'power through' pain until your body gives out. Sad.
Asset Finance Komrade
December 16, 2025
Interesting analysis. But one must question the underlying assumption: that swelling is inherently pathological. In evolutionary terms, fluid retention may be a protective mechanism-perhaps the body is attempting to buffer toxin exposure or modulate inflammatory response. The medical model treats swelling as a failure, when it may be a sophisticated adaptation.
Furthermore, the suggestion to switch from amlodipine to losartan ignores pharmacogenetic variability. In some populations, particularly those of East Asian descent, ARBs carry higher risks of angioedema. A blanket recommendation is dangerous.
And while compression stockings help, they're a Band-Aid on a systemic issue. The real solution? Decentralize healthcare. Let patients choose their own risk thresholds. Not every 15% chance of swelling warrants a drug switch. Some would rather have controlled edema than uncontrolled hypertension.
Also, emoji: 🧂🩸🦵
Brianna Black
December 17, 2025
As a nurse who's worked in oncology for 18 years, I've seen hand-foot syndrome turn patients into recluses. One woman cried because she couldn't hold her granddaughter's hand. That's not just side effect-that's loss of humanity. We treat the cancer, but we forget the person. This post? It's a lifeline. I print it out and hand it to every new patient starting capecitabine. They don't know what to expect. They think it's just 'bad skin.' It's not. It's a signal. And we owe it to them to speak up. Thank you for writing this. I'm sharing it with every department.
Write a comment