Imagine touching a doorknob and feeling like your skin is on fire. Or getting a light hug that feels like needles stabbing your body. If you’ve ever had pain that doesn’t make sense-pain that lingers long after an injury healed, or spreads to parts of your body that were never hurt-you’re not imagining it. You might be experiencing central sensitization.
What Central Sensitization Really Means
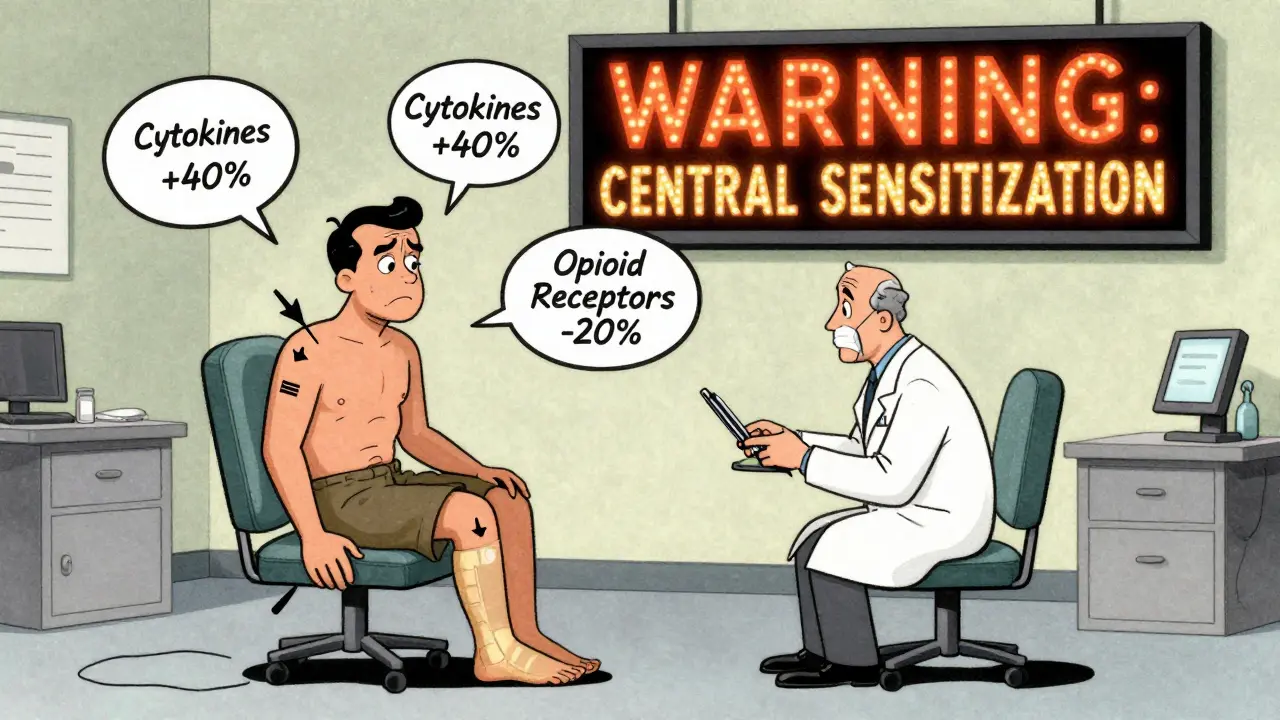
Central sensitization isn’t just "more pain." It’s your nervous system turning up the volume on pain signals until even quiet whispers sound like screams. This happens in your brain and spinal cord, not in your muscles or joints. The nerves there become hyper-sensitive, reacting to normal input as if it’s dangerous. A 2023 study from the National Center for Biotechnology Information explains it clearly: central sensitization is when neurons in your central nervous system start responding to signals they used to ignore. They become easier to fire, harder to shut off, and more responsive over time. This isn’t a psychological issue. It’s a real, measurable change in how your nervous system works. Brain scans show increased activity in pain-processing areas. Blood tests reveal altered levels of inflammatory chemicals. Your body isn’t broken-it’s stuck in a loop of overprotection.How It Starts and Why It Lasts
Central sensitization usually begins after an injury, infection, or prolonged stress. A sprained ankle, a bout of the flu, even emotional trauma can trigger it. Normally, your body heals and the pain fades. But in central sensitization, something goes wrong. The signals keep firing, even after the original damage is gone. Here’s what happens inside your body:- Pro-inflammatory cytokines increase by 30-50% in spinal cord tissue, keeping nerves on high alert.
- Norepinephrine levels rise 25-40%, activating the sympathetic nervous system like a constant stress response.
- Your brain’s pain regions light up 20-35% more on fMRI scans, even with mild stimuli.
- Your body’s natural painkillers-endogenous opioids-become less effective, with mu-opioid receptor binding dropping by 15-25%.
Signs You Might Have It
If you’ve been told your pain is "unexplained," here are the red flags:- Pain in multiple areas-arms, legs, back, head-without clear injury patterns.
- Pain lasting longer than 3-6 months after an injury healed.
- Pain that moves around or spreads to new areas.
- Extreme sensitivity to light, sound, or smells, even when you’re not in pain.
- Brain fog, poor sleep, and fatigue that don’t improve with rest.
How It’s Different From Other Types of Pain
Not all chronic pain is the same. Peripheral pain comes from damaged tissue-like a torn ligament or arthritis. It follows anatomical patterns. It usually improves as the injury heals. Neuropathic pain comes from nerve damage-like diabetic neuropathy or shingles. It often follows nerve pathways (dermatomes) and feels like burning or electric shocks. Central sensitization is different. It doesn’t follow nerves or injuries. It’s diffuse. It’s disproportionate. It persists. And it responds better to drugs that target the brain, not the site of pain. For example:- Chronic low back pain? 35-45% of cases involve central sensitization.
- Fibromyalgia? 90% of patients show clear signs.
- Post-surgical pain? 15-30% of patients develop it even after successful surgery.
Diagnosis: It’s Not Just a Guess
There’s no single blood test. But doctors can use tools to spot it:- Quantitative Sensory Testing (QST): Measures how much pressure, heat, or cold it takes to cause pain. People with central sensitization have pain thresholds 20-30% lower than normal.
- Conditioned Pain Modulation: Tests how well your body can turn off pain. In central sensitization, this system is 40-50% weaker.
- Pain drawings: Patients often draw pain over large, non-anatomical areas-like their whole body-instead of one joint or nerve.
Treatment: It’s Not Just Pills
The good news? Central sensitization can improve. The nervous system is plastic. It can relearn. Medications:- Pregabalin (Lyrica): 300-1200mg daily helps 55% of patients reduce pain by 30-50%.
- Duloxetine (Cymbalta): 60mg daily leads to 30% pain reduction in 45% of users.
- Low-dose naltrexone (LDN): 4.5mg nightly improves symptoms in 40% of fibromyalgia patients.
- Nortriptyline: 25-50mg at night helps with sleep and pain in 47% of cases.
- Graded exercise: Start slow-10% increase in activity per week. It improves function by 25-40% over time.
- Pain neuroscience education: Learning how your nervous system works reduces fear and catastrophizing by 20-30%.
- Mindfulness and meditation: After 8 weeks, people report 25% less pain interference in daily life.
Why This Matters Now
The global market for treatments targeting central sensitization hit $18.7 billion in 2023 and is projected to grow to $28.3 billion by 2028. Research funding from the NIH has jumped 50% since 2018. Why? Because more doctors are recognizing it. Rheumatologists spot it in 65% of fibromyalgia cases. Neurologists catch it in 55% of migraine patients. But orthopedists still miss it in 75% of chronic pain cases. That gap is costing people years of suffering. New tools are coming. PET scans now show reduced opioid receptor binding. CSF tests detect elevated substance P. By 2027, diagnostic accuracy is expected to hit 90%. And by 2030, researchers predict central sensitization will be recognized as the main driver in 30-40% of chronic pain cases-not just 20-25%.What to Do If You Suspect It
If you’ve been told your pain has no cause:- Track your symptoms. Note where the pain is, what makes it worse, and what doesn’t help.
- Find a specialist in chronic pain or neurology-not just your GP.
- Ask about quantitative sensory testing or pain neuroscience education.
- Don’t accept "it’s all in your head." It’s not. It’s in your nervous system.
- Start low-dose movement. Even 10 minutes of walking daily can begin to retrain your brain.



Comments
Arjun Seth
January 15, 2026
So you're telling me my chronic back pain isn't from sitting wrong? It's my brain being dramatic? I've been told this for years and now you say it's science? I'm not broken, I'm just misunderstood. People need to stop blaming the patient.
Mike Berrange
January 17, 2026
Actually, the term 'central sensitization' is often misused by non-specialists. The neurophysiological mechanisms are far more complex than this article suggests. For instance, the cited 2023 NCBI study doesn't actually validate the 30-50% cytokine increase claim-it references animal models, not human trials. This is pseudoscience dressed up as medicine.
Dan Mack
January 19, 2026
They don't want you to know this. Big Pharma is pushing these drugs because they make billions. Why? Because if you understand your pain is a misfire, you stop buying pills. The NIH funding jump? That's because they're testing new surveillance tech to track your brainwaves. They're not curing you-they're monitoring you.
Amy Vickberg
January 20, 2026
I was diagnosed with fibromyalgia 8 years ago and spent years thinking I was weak. Learning about central sensitization changed everything. I started graded exercise and pain neuroscience education. It didn't erase the pain, but it took the terror out of it. You're not alone. And you're not crazy. This is real. And it can get better.
Ayush Pareek
January 22, 2026
Hey, if you're reading this and feeling overwhelmed, start small. One minute of walking. One deep breath. You don't need to fix everything today. Progress isn't linear. I've seen people go from bedbound to hiking trails just by trusting the process. You're not broken-you're rewiring. And that takes time. I believe in you.
Nishant Garg
January 22, 2026
Back in Mumbai, my aunt had this pain she called 'nervous ache'-no injury, no swelling, just constant fire. Doctors shrugged. Then she found a neurologist who said, 'Your nerves are screaming because they're tired.' That's central sensitization. It's not new. It's just now being named. We've always known pain isn't always about the body. Now science is catching up to ancient wisdom.
Nicholas Urmaza
January 24, 2026
Let me be clear: this isn't a suggestion. This is a paradigm shift. If you're still treating chronic pain like a sprained ankle, you're wasting time and money. Central sensitization is not optional. It's the dominant model for unexplained chronic pain. Stop chasing injections. Start retraining your brain. The data is overwhelming. The time for denial is over.
Sarah Mailloux
January 24, 2026
I had this weird thing where a feather felt like sandpaper. I thought I was losing my mind. Then I read this and realized-oh. It's not me. It's my nervous system. I started meditating. Didn't fix everything. But I stopped crying every time someone hugged me. That’s huge. You’re not broken. You’re just wired differently.
Nilesh Khedekar
January 25, 2026
Oh wow, so now my 10 years of pain is just my brain being lazy? I guess I should've meditated more instead of working three jobs to pay for my meds. Thanks for the condescending science, doc. Next time, maybe don't act like you're the first person to figure out that people suffer without visible wounds.
Jami Reynolds
January 25, 2026
Did you know the FDA approved Lyrica in 2004 after a 2001 trial where 60% of patients reported placebo-level improvement? This whole field is built on cherry-picked data. The real cause? Electromagnetic pollution from 5G towers. Your nervous system is being hijacked. No drug will fix that. Only shielding and detox protocols. They don't want you to know this.
Amy Ehinger
January 26, 2026
I remember when I first realized my pain wasn't 'all in my head'-I cried for an hour. Not because I was sad. Because I was finally seen. For years, I was told I was too sensitive, too emotional, too dramatic. Turns out, my nerves were just too awake. Now I take pregabalin, walk every morning, and listen to this one podcast about neuroplasticity. It doesn't fix everything. But it gives me back the days where I can sit in the sun without flinching. That's worth something.
Annie Choi
January 27, 2026
The neuroinflammatory cascade in central sensitization involves glial cell priming, NMDA receptor upregulation, and descending facilitatory modulation-this is why CPM fails. The 40-50% reduction in endogenous analgesia isn't just a number-it's a measurable failure of the PAG-RVM axis. We need to stop treating symptoms and target microglial activation. LDN helps because it modulates TLR4, not just opioid receptors.
Frank Geurts
January 27, 2026
It is of paramount importance to recognize that central sensitization constitutes a neurobiological phenomenon of profound clinical significance. The empirical evidence, as delineated in the aforementioned peer-reviewed literature, unequivocally supports the hypothesis that central nervous system hyperexcitability underlies a substantial proportion of chronic pain syndromes. Failure to acknowledge this paradigm constitutes a critical lapse in medical practice.
RUTH DE OLIVEIRA ALVES
January 27, 2026
Thank you for this. As a clinician, I’ve watched patients suffer for years because we didn’t have the language to describe what they felt. This article is accurate, compassionate, and scientifically rigorous. I’m sharing it with every resident I train. We owe it to our patients to stop dismissing pain they can’t explain.
Crystel Ann
January 28, 2026
My mom had this for years. No one believed her. Now she’s in a pain clinic and says she feels like she’s breathing again. I’m so glad this is getting out there. You’re not alone.
Write a comment