Why Rural Patients Need Better Side Effect Monitoring
Living far from a hospital doesn’t just mean longer drives-it means delayed care when something goes wrong with your medication. In rural areas, patients taking blood thinners, antidepressants, or high blood pressure drugs are 23% more likely to suffer preventable side effects than those in cities. Many don’t know they’re at risk until it’s too late. A tremor, a dizzy spell, or unusual bruising might be ignored because the nearest clinic is two hours away. By then, a minor reaction could become a hospital emergency.
Telehealth isn’t just a convenience for rural patients-it’s a lifeline. With real-time monitoring, side effects like high INR levels from warfarin or serotonin syndrome from SSRIs can be caught before they turn dangerous. A patient in Montana used a Bluetooth-connected INR monitor to spot a dangerous spike in blood clotting levels before symptoms appeared. That early warning prevented a life-threatening bleed. This isn’t rare. Studies show telehealth monitoring cuts hospitalizations for medication side effects by 31% in rural communities.
How Telehealth Monitoring Actually Works
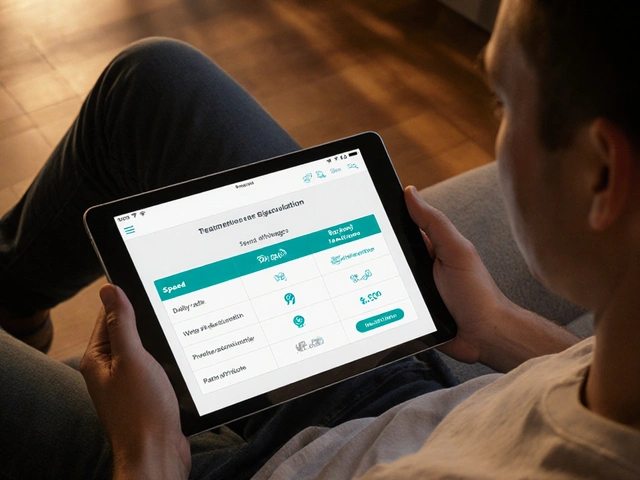
It’s not just video calls. Modern telehealth side effect monitoring combines devices, apps, and human follow-up into a system that works like a safety net. Patients use FDA-cleared devices to track vital signs: blood pressure cuffs, heart rate monitors, or smart inhalers that log usage. Some take a daily photo of their skin for rashes or swelling. Others use smart pill dispensers that alert providers when a dose is missed.
These tools sync with secure apps that patients open once a day. They answer simple questions: “Did you feel dizzy today?” “Any nausea?” “How’s your sleep?” The system flags red flags automatically-like a sudden drop in blood pressure or repeated reports of confusion. Nurses or pharmacists review alerts and reach out within hours, not days.
For patients without smartphones, audio-only calls are now covered by Medicare. A simple phone call can catch symptoms like swelling in the legs or worsening depression. One program in West Virginia uses automated voice prompts to check in with seniors. If a patient doesn’t respond after three attempts, a nurse calls. That’s how they found an 82-year-old woman whose new anticoagulant had caused internal bleeding-she didn’t realize it was serious until the call came.
What Works Best: Tools and Tech That Deliver
Not all telehealth tools are created equal. The most effective programs use a mix of hardware, software, and human support.
- Bluetooth INR monitors for blood thinners: Used in 92% of successful anticoagulation programs. Patients prick their finger at home; results send automatically to their care team.
- Smart pill dispensers like Hero Health: Detect missed doses with 85% accuracy. Send alerts to both patient and provider.
- Wearable sensors: New pilot programs in Arkansas use wristbands to detect movement changes caused by antipsychotic drugs-like tardive dyskinesia-before doctors can see them.
- AI-powered alerts: IBM Watson’s MedSafety system analyzes symptoms and lab trends to predict side effects 48 hours in advance with 84% accuracy.
These tools only work if they’re integrated. The best programs connect directly to electronic health records like Epic or Cerner. That way, when a patient reports nausea, their provider sees it alongside their latest lab results and medication list-all in one place.
Barriers That Still Block Access
Even with great tech, many rural patients can’t use it. About 28% of rural Americans don’t have broadband that meets federal standards. In some areas, the only reliable internet is on a cell tower ten miles away. A patient in Montana told a researcher: “I have to drive to the library to upload my blood pressure readings.”
Then there’s the learning curve. Older adults need an average of 3.2 training sessions just to use the app. Many struggle with small buttons, confusing menus, or voice recognition that doesn’t understand their accent. One West Virginia patient said: “The video was so pixelated, my doctor couldn’t see my shaking hands.”
Health literacy is another hurdle. One in three rural adults can’t read medical instructions well. If a patient doesn’t understand what “dizziness” or “bradycardia” means, they won’t report it. Programs that succeed use plain language, pictures, and bilingual staff. A clinic in New Mexico uses Spanish-language videos to explain how to use a blood pressure cuff. Their adherence rate jumped from 58% to 88%.
Who’s Running These Programs Successfully?
The most effective telehealth side effect programs don’t just hand out devices-they build relationships.
The University of Mississippi Medical Center runs a program for patients on warfarin. They pair each patient with a pharmacist who does weekly video visits. Patients use a Bluetooth INR monitor. The pharmacist reviews trends, adjusts doses, and answers questions. Retention? 92%. Hospitalizations? Down 40%.
Another model: pharmacist-led monitoring. The American Pharmacists Association found these programs achieve 89% medication adherence-compared to 62% in traditional care. Pharmacists know drugs inside out. They spot patterns a busy doctor might miss. A 2024 study from Vanderbilt showed adding pharmacists to telehealth teams cut severe side effects by 43%.
Success also depends on staff. Rural clinics are short on nurses and care coordinators. The best programs assign one person to manage telehealth monitoring full-time. That person trains patients, reviews alerts, calls at-risk patients, and coordinates with doctors. Without that role, alerts pile up-and patients fall through the cracks.
What’s Changing in 2026
Policy is catching up. In January 2024, Medicare started paying $27 per day for asynchronous monitoring-meaning patients can send updates anytime, and providers get paid to review them later. This makes it easier for clinics to scale without needing staff on call 24/7.
The FCC is spending $20.4 billion through 2025 to fix rural internet. New towers and fiber lines are coming to places that haven’t had reliable service in decades. That’s a game-changer for telehealth.
Pharmaceutical companies are also stepping in. Pfizer and Merck have invested $450 million since 2022 to fund telehealth adherence programs for rural patients. They’re not doing it out of charity-they’re reducing costly hospitalizations tied to poor medication management.
But there’s a catch. When big urban telehealth companies set up shop in rural areas, they often draw patients away from local clinics. That cuts into the revenue those clinics need to stay open. A 2023 study showed rural hospital margins dropped 8% when outside telehealth providers entered the market. The solution? Keep monitoring local. Train rural nurses. Pay rural pharmacists fairly. Support community-based care.
What Patients Are Saying
“The app caught my INR going high before I felt anything. I didn’t even know I was at risk.” - Montana patient, r/telehealth
“I used to drive 90 miles every week for my blood pressure check. Now I do it in my kitchen. I’ve saved 3,000 miles in two years.” - Iowa woman on Medicare
“The video call was so glitchy, I couldn’t show my doctor the rash. I had to drive in anyway.” - West Virginia patient, Healthcare.gov review
“I didn’t know what ‘bradycardia’ meant. The nurse drew me a picture of a heart and circled the slow beats. That’s when it clicked.” - Rural Ohio senior
Eighty-two percent of rural patients say telehealth side effect monitoring is “very” or “extremely” helpful. But 41% still report tech problems. The gap isn’t in the tools-it’s in the support.
How to Get Started
If you’re a rural patient or caregiver:
- Ask your provider: “Do you have a telehealth program for monitoring side effects?”
- Find out what tools they use. Ask if they offer audio-only options if video doesn’t work.
- Request training. Don’t be afraid to ask for extra help. Most programs offer at least two sessions.
- Use the app every day-even if you feel fine. Consistency saves lives.
- Report anything unusual. Even if you think it’s “just a headache.”
If you’re a provider or clinic:
- Start small. Pick one high-risk medication-like warfarin or antidepressants-and build a program around it.
- Partner with a pharmacist. They’re the secret weapon.
- Use plain language and visuals. Avoid medical jargon.
- Train staff to follow up. A missed call = a missed warning.
- Advocate for fair reimbursement. Push insurers to match Medicare’s $51/20-minute rate.
Final Thought: It’s Not About Tech-It’s About Trust
Telehealth won’t fix rural healthcare if it feels cold or impersonal. The magic happens when a nurse remembers your name, checks in because your last INR was high, and asks, “How’s your granddaughter doing?” That’s what keeps people coming back. Technology gives us the tools. Human connection gives us the trust. And trust is what keeps patients alive.



Comments
Laura Arnal
January 30, 2026
This is literally life-saving stuff. I’ve been using a Bluetooth INR monitor for my warfarin, and honestly? I don’t know how I ever lived without it. My nurse gets my readings automatically, and last month she caught my levels creeping up before I even felt dizzy. 🙌 No more 2-hour drives just to get a blood test. Rural folks deserve this kind of care, not just lip service.
Jasneet Minhas
January 31, 2026
Ah yes, the classic tech solution to a systemic problem. 🤖📱 We’ll give you a $300 smart pill dispenser but still won’t fix the 40-minute wait for a GP in your county. Also, ‘plain language’? Try translating ‘bradycardia’ into the dialect spoken in Appalachia. Good luck with that. 😅
Eli In
February 2, 2026
I’m from a tiny village in New Mexico, and our clinic started using Spanish-language video guides for meds last year. My abuela finally understands her blood pressure meds now-she used to skip doses because she thought ‘hypertension’ meant she had too much coffee. 🌺 The picture of the heart with the slow beat? That’s magic. We don’t need fancy AI. We need people who listen.
Paul Adler
February 3, 2026
The data here is compelling, particularly the 31% reduction in hospitalizations. However, one must consider the infrastructure prerequisites: reliable broadband, digital literacy, and consistent human oversight. Without these, even the most advanced telehealth platform becomes a digital placebo. The integration with Epic and Cerner is non-negotiable for scalability and safety.
Write a comment