Every day, pharmacists make critical decisions about generic medications-decisions that can affect patient safety, cost, and treatment outcomes. With over 90% of prescriptions filled with generics in the U.S., and new generic approvals rising by 17% year-over-year, staying up to date isn’t optional. It’s a daily requirement. Yet many pharmacists still struggle with outdated training, confusing state rules, and rapidly changing bioequivalence standards. If you’re a pharmacist wondering how to keep your generics knowledge sharp without drowning in boring online modules, here’s what actually works.
Why Generics Training Isn’t Just Another CE Box to Check
Continuing education for pharmacists isn’t about ticking a box. It’s about preventing errors. In 2021, ACPE found that 42.7% of all pharmacy malpractice claims involved mistakes related to generic substitution or misunderstanding therapeutic equivalence ratings. That’s not a small risk. It’s a systemic one.
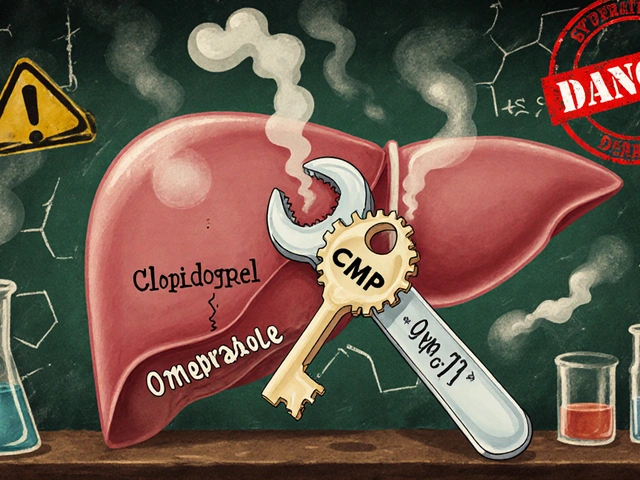
Take levothyroxine, for example. Even small differences in bioavailability between generic brands can cause serious thyroid issues. The FDA requires generics to be within 80-125% of the brand drug’s absorption rate, but that range still leaves room for error-especially when switching between multiple generic manufacturers. Pharmacists who completed at least five hours of targeted generics training each year made 37% fewer substitution errors, according to the American Pharmacists Association. That’s not theory. That’s real-world impact.
And it’s not just about dosage. It’s about the legal side too. The CREATES Act, state-specific substitution laws, and patent litigation have turned generic prescribing into a minefield. One pharmacist in Texas told me she lost a license review because she didn’t know her state banned automatic substitution for narrow therapeutic index drugs like warfarin. She’d never been trained on it. That’s not negligence-it’s a gap in the system.
What the Law Actually Requires (And How It Varies)
All 50 U.S. states require pharmacists to complete continuing education to renew their license. The hours range from 15 to 30 every two years. But here’s the catch: what counts varies wildly.
In Illinois, you need 30 hours every two years-including one hour each on sexual harassment prevention, implicit bias, and, starting January 1, 2025, cultural competency. In California, you don’t submit your CE certificates unless audited, but you must keep them for two years. In New York, you have to mail in proof with your renewal application. One wrong step, and your license renewal gets delayed.
And then there’s the generics-specific stuff. Only 12 states require dedicated biosimilar training. Eighteen require opioid alternative education-which often includes generic options. Seven have special rules for narrow therapeutic index drugs. If you practice in more than one state, you’re juggling five different sets of rules. No wonder pharmacists feel overwhelmed.
ACPE-accredited courses are your safest bet. They’re the only ones that count across state lines. Look for courses labeled “ACPE #” with a number. Avoid anything labeled “for credit only” or “self-study without assessment.” Those won’t pass audit.
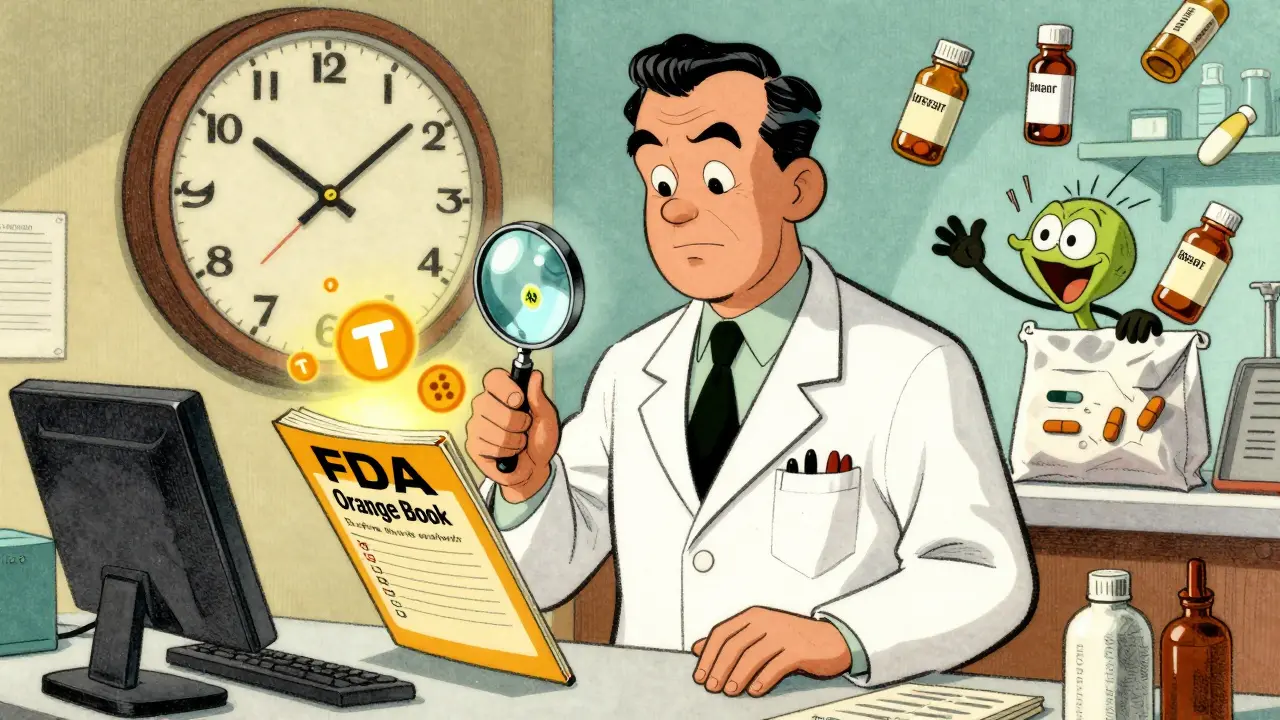
The FDA Orange Book: Your Most Important Tool (And How to Use It)
The FDA Orange Book is the bible for generic substitution. It lists every approved generic drug and assigns a therapeutic equivalence rating-TE codes like AB, BX, or AE. AB means interchangeable. BX means not rated. AE means equivalent but with special conditions.
Here’s what most pharmacists miss: these ratings change monthly. The FDA approves nearly 1,000 new generic applications each year. That means a drug you thought was AB-rated last month might now be BX because the manufacturer changed its formulation. If you don’t check the Orange Book before dispensing, you’re guessing.
Dr. John Smith from the University of Illinois College of Pharmacy says pharmacists need to know over 1,200 TE codes. That’s not something you memorize. It’s something you learn how to look up quickly. The best CE courses don’t make you memorize codes-they teach you how to use the FDA’s online database, how to spot red flags in substitution alerts, and when to consult the prescriber.
Pro tip: Bookmark the FDA’s Orange Book site. Set a monthly calendar reminder to check for updates on the top 10 generics you dispense most. That’s 20 minutes a month. It’s cheaper than a malpractice claim.

What Kind of CE Actually Works (And What’s a Waste of Time)
Not all continuing education is created equal. Knowledge-based courses-where you watch a video and answer multiple-choice questions-are easy to complete. But they’re also easy to forget.
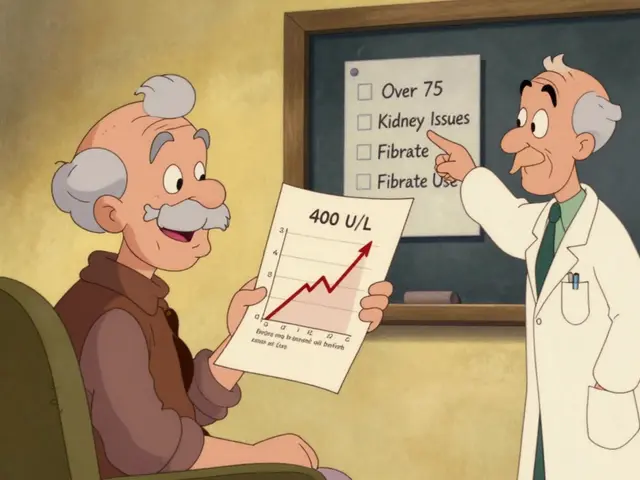
Pharmacists who took application-based courses with real case studies rated them 4.7 out of 5. Those who took basic lectures gave them 3.2. Why? Because they actually used the knowledge.
For example, a good case study might say: “A 68-year-old with atrial fibrillation was switched from brand-name warfarin to a generic. INR spiked to 6.2. What went wrong?” The answer isn’t just “the generic was weaker.” It’s about bioequivalence ranges, patient history, and whether the pharmacy had a substitution policy. That’s learning that sticks.
Top providers like Pharmacist’s Letter and PocketPrep offer free, ACPE-accredited modules focused on real-world scenarios. PocketPrep’s user base grew 32% in 2023-mostly because pharmacists kept coming back for the case-based quizzes. If you’re choosing between a 2-hour lecture and a 90-minute case review, pick the case study every time.
Biosimilars Are the New Frontier (And Most Pharmacists Are Behind)
Biosimilars aren’t generics. They’re complex biological drugs that mimic brand-name biologics like Humira or Enbrel. But they’re still treated like generics in many pharmacies-and that’s dangerous.
The ASHP 2023 survey found 78% of hospital pharmacists felt unprepared to handle biosimilar interchangeability. Why? Because the rules are different. Unlike small-molecule generics, biosimilars require FDA approval for interchangeability, and not all are designated as such. Even then, some states require prescriber authorization before substitution.
ACPE announced new standards in January 2024: all generics-related CE must include biosimilar interchangeability and REMS program training starting January 1, 2025. If your current CE provider hasn’t updated their curriculum, you’re at risk of falling out of compliance.
Don’t wait. Find a course that covers: FDA’s interchangeability criteria, REMS requirements, and state laws on biosimilar substitution. If you’re dispensing these drugs, you need to know them.

How to Build a Sustainable Generics Learning Habit
You don’t need to spend 30 hours a year on generics. You need to spend 10 minutes a week.
Here’s a simple system:
- Every Monday, spend 10 minutes checking the FDA Orange Book for updates on your top 5 most-prescribed generics.
- Every month, complete one 60-minute ACPE-accredited case study (many are free).
- Every quarter, review your state’s pharmacy board website for new CE rules.
- Every year, take one 2-hour course on biosimilars or narrow therapeutic index drugs.
That’s 10 hours a year. Less than half the average requirement. And you’ll be ahead of 80% of your peers.
Use tools like PocketPrep or Pharmacist’s Letter to get alerts when new TE codes are published. Set up Google Alerts for “FDA generic approval” and “state pharmacy substitution law.” Keep a simple spreadsheet: Drug Name, TE Code, Last Checked, Notes. It takes 5 minutes. It saves lives.
What’s Coming Next (And How to Prepare)
The future of pharmacy CE is personalized. AI-powered platforms are starting to analyze your dispensing history and flag knowledge gaps. CVS Health piloted a system that pushed just-in-time learning to pharmacists right before they dispensed a high-risk generic-reducing errors by 28%.
By 2027, IQVIA predicts 35% of CE will be delivered this way. That means your next CE module might say: “You dispensed three different levothyroxine generics last month. Here’s a 10-minute update on the latest bioequivalence data.”
Don’t wait for the future. Start building your own system now. Track your own errors. Ask colleagues what tripped them up. Join a pharmacy forum like r/pharmacy on Reddit. Read the monthly updates from ASHP and NABP. The information is out there. You just need to make time for it.
Generics aren’t going away. They’re growing. And the people who stay current won’t just meet their CE requirements-they’ll become the pharmacists other pharmacists turn to for advice. That’s not just professional growth. That’s professional power.
Do I need separate CE for each state I’m licensed in?
Yes. If you hold licenses in multiple states, you must meet each state’s CE requirements. Some states accept ACPE credits across borders, but others have unique mandates-like Texas’s rules on narrow therapeutic index drugs or New York’s submission rules. Always check your state board’s website before completing any course. Keep records for at least two years, even if your state doesn’t require submission.
Are free CE courses accredited and accepted?
Yes, if they’re ACPE-accredited. Providers like Pharmacist’s Letter and the American Pharmacists Association offer free, accredited courses that count toward license renewal. Look for the ACPE course number (e.g., ACPE #0012-9999) on the course page. If it’s not there, it’s not accredited. Free doesn’t mean low quality-many of the best case studies are free.
What’s the difference between a generic and a biosimilar?
Generics are chemically identical copies of small-molecule drugs, like metformin or lisinopril. Biosimilars are highly similar versions of complex biological drugs, like insulin or monoclonal antibodies. They’re not exact copies due to their complexity. Only biosimilars designated as “interchangeable” by the FDA can be substituted without prescriber approval-and even then, state laws may require authorization. Never assume a biosimilar is interchangeable unless it’s clearly labeled as such.
How often should I check the FDA Orange Book?
At least once a month. The FDA updates therapeutic equivalence ratings monthly. If you dispense high-risk drugs like levothyroxine, warfarin, or seizure medications, check weekly. Set a calendar reminder. Use the FDA’s searchable database-it’s free and updated in real time. Don’t rely on old printouts or outdated apps.
Can I use CE from non-accredited providers?
No. Only ACPE-accredited or state board-approved courses count toward license renewal. Many online platforms offer “CE credits” that aren’t recognized. Always verify the provider is listed on the ACPE website or your state board’s approved list. If you’re unsure, call your state board. It’s better to be safe than to have your renewal denied.


Comments
Brian Furnell
December 21, 2025
Let’s be real-most CE courses are glorified PowerPoint death marches. But the Orange Book? That’s the actual Bible. I check it every Monday morning with my coffee. If you’re not tracking TE code changes, you’re flying blind. AB to BX can happen overnight, and if you don’t catch it, you’re one step away from a malpractice call.
ACPE credits are non-negotiable. I’ve seen pharmacists get audited because they took some ‘free CE’ from a sketchy site that didn’t even have an ACPE number. Don’t be that person. Save yourself the headache.
And biosimilars? Jesus. I had a nurse ask me why we couldn’t just swap Humira for the biosimilar like it was ibuprofen. We had to do a full 20-minute consult. It’s not a generic. It’s a whole different beast. The FDA’s interchangeability criteria are a maze, and most states haven’t caught up yet.
Set up Google Alerts for ‘FDA generic approval’ and ‘biosimilar substitution law.’ I did. Got a notification last month about a new AB rating for levothyroxine-changed my entire dispensing protocol. Ten minutes a week. That’s it. That’s the whole game.
And stop using outdated apps. I still see people using the 2019 version of the Orange Book app. It’s like using a rotary phone in 2024. The FDA’s site is free, updated hourly, and searchable. Use it.
Case studies > lectures. Always. I took a PocketPrep module last week on warfarin switching-real patient, real INR spike, real consequences. I still think about it. That’s learning. Not memorizing multiple-choice answers while scrolling TikTok.
States are a nightmare. I’m licensed in NY and PA. NY wants mailed proof. PA doesn’t care until you’re audited. And Texas? Don’t even get me started. One wrong substitution on a narrow TI drug and you’re in front of the board. Keep a spreadsheet. I have one. Drug, TE code, last checked, notes. Five minutes. Life saver.
ACPE-accredited courses are the only thing that cross state lines. If it doesn’t have a number, it doesn’t count. Period. I’ve had to retake courses because I didn’t verify. Don’t make my mistake.
And for the love of God, stop assuming biosimilars are interchangeable. Just because it’s ‘similar’ doesn’t mean it’s substitutable. I’ve seen pharmacists get fired for that. Read the label. Read the state law. Read the REMS. Triple-check.
It’s not about ticking boxes. It’s about not killing someone because you didn’t check a database. That’s the bottom line.
Siobhan K.
December 21, 2025
So let me get this straight-you’re telling me the entire pharmacy profession is being held hostage by a 30-year-old government database that updates monthly, and the solution is to spend 10 minutes a week staring at it? Brilliant.
Meanwhile, the FDA approves a new generic every 10 minutes, states change their rules like fashion trends, and we’re supposed to memorize 1,200 TE codes? No. We’re supposed to be smart enough to look them up. That’s the whole point of digital tools.
But no. We need another 2-hour webinar where someone reads off a script while we half-listen between sips of cold coffee. And then we get audited because we didn’t submit a certificate we didn’t even know we had to keep.
The real problem isn’t that pharmacists are lazy. It’s that the system is designed to make us feel guilty for not being superhumans. You don’t need a spreadsheet. You need a system that doesn’t require you to be a full-time compliance officer on top of your actual job.
And yet here we are. Still checking the Orange Book like it’s the Dead Sea Scrolls. The FDA should just send a weekly email. Or better yet-integrate the TE codes into our dispensing software. But no. That would be too easy. We’d rather have 50 different state rules and 10,000 confused pharmacists.
It’s not education. It’s bureaucratic performance art.
Sandy Crux
December 21, 2025
How quaint. You assume pharmacists care about TE codes. Most of them are just glorified pill counters who haven’t read a journal since residency. The Orange Book? Most don’t even know it exists. They rely on the pharmacy software’s auto-substitute feature-blindly. And if it’s flagged? They just click ‘override’ and move on.
And biosimilars? Please. Half the pharmacists I’ve worked with think ‘biosimilar’ is just a fancy word for ‘generic.’ They don’t understand immunogenicity. They don’t know what REMS is. They don’t care. They’re paid by the script, not by the outcome.
CE courses? They’re a joke. The same three providers dominate the market, charging $200 for content that’s 80% recycled from last year’s lecture. The FDA doesn’t even require CE to be relevant-just ‘accredited.’
And yet you praise PocketPrep? As if gamified quizzes are the answer to systemic incompetence. It’s not about learning. It’s about compliance theater. We’re not training pharmacists. We’re training them to pass audits.
The real solution? Remove CE requirements entirely. Let pharmacists self-direct their learning. Or better yet-hold manufacturers accountable for clear labeling and standardized substitution rules. But that would require regulation. And we all know how much we love that.
Until then, keep your spreadsheets. I’ll be over here, dispensing drugs while wondering why we still live in the Stone Age.
Hannah Taylor
December 23, 2025
ok so here’s the thing i think the whole generics thing is a big pharma scam. they make the brand name drug super expensive so people switch to generic then they make the generic with slightly different filler so it doesn’t work as good and then they charge more for the new version and we all get confused and some old lady dies from levothyroxine and no one cares. the orange book? lol i bet they change it to trick us. i heard the fda is owned by pfizer. and state laws? they’re just there to keep us busy. why do we even need ce? just let pharmacists do their job. they’re not robots. stop making us check a website every week. it’s too much. i just want to give people their meds without thinking about te codes. it’s 2024. why is this still a thing?
mukesh matav
December 24, 2025
Respectfully, I’ve seen this play out in rural India too-where generics are the only option. But here, the issue isn’t just education. It’s access. In many places, pharmacists don’t have internet. They don’t have updated software. They rely on paper guides from 2012.
So when you talk about the FDA Orange Book, I hear you. But I also hear a system designed for urban, tech-savvy pharmacies. What about the ones in villages where the nearest pharmacy is 30 miles away and the pharmacist is the only trained person for 50 kilometers?
Maybe the real solution isn’t more CE. Maybe it’s better labeling. Or a simple QR code on every generic package that links to the current TE rating. No internet? No problem. Scan with a phone. Done.
And biosimilars? In India, they’re not even regulated properly. We don’t have ACPE. We have a patchwork of state boards that barely function. So yes, I agree with the system. But I also pity the people trying to survive it.
Education matters. But infrastructure matters more.
Peggy Adams
December 25, 2025
i swear to god if i have to do one more ce course where some guy in a blazer talks about 'therapeutic equivalence' while i'm eating my lunch i'm gonna quit. who even cares if a generic is ab or bx? if the patient feels fine, they're fine. they don't know the difference. why are we making this so complicated? just give them the cheapest thing on the shelf. the fda is full of bureaucrats who don't even know how to fill a prescription. stop overthinking it.
Jay lawch
December 26, 2025
Let me tell you something about the American healthcare system. It is not broken. It is working exactly as intended. The FDA, the ACPE, the state boards-they are all components of a grand machine designed to keep the masses docile, distracted, and obedient.
Generics? They are not cheaper. They are a psychological tool. The pharmaceutical industry wants you to believe that generics are safe, so you don’t question the pricing of the brand. But they are not identical. They are not. They are chemically similar, yes-but the fillers, the binders, the coatings-they are all different. And they matter. But you are not allowed to know that. Because if you knew, you might stop taking the drugs altogether.
And the Orange Book? A mirage. A distraction. A false sense of security. The FDA updates it monthly? Yes. But who is updating it? Who is auditing the manufacturers? Who is ensuring that the bioequivalence studies are not falsified? You think they are honest? You think they are transparent?
They are not. They are corporate puppets. And CE courses? They are not education. They are indoctrination. They teach you to trust the system. To follow the rules. To check the website. To fill out the forms. To become a cog.
But I am not a cog. I am a man. And I refuse to be programmed. I will not check the Orange Book. I will not take the ACPE course. I will not pretend that this system is about patient safety. It is about profit. And control.
And if you think otherwise, you are part of the machine.
Christina Weber
December 28, 2025
It’s not that pharmacists are lazy-it’s that the entire system is catastrophically misaligned. You cite ACPE accreditation as the gold standard, but ACPE is a private, for-profit entity that charges pharmacies hundreds of dollars for each course. Meanwhile, the FDA’s Orange Book is free, publicly accessible, and updated in real time-and yet it’s ignored because no one taught pharmacists how to use it properly.
There’s a reason why 42.7% of malpractice claims involve generics: because pharmacists are trained to follow software prompts, not clinical judgment. The CE industry profits from creating artificial complexity. Case studies? Great. But why are they not mandatory? Why are they expensive? Why are they buried under 20 other courses that are just video lectures with multiple-choice questions?
And biosimilars? The fact that 78% of hospital pharmacists feel unprepared is not a CE failure. It’s a regulatory failure. The FDA should have mandated standardized training before approving the first biosimilar. But they didn’t. And now we’re patching the hole with more paperwork.
Stop glorifying PocketPrep. It’s a band-aid. The real solution is to eliminate redundant CE requirements and replace them with mandatory, competency-based assessments tied to actual dispensing patterns. But that would require data transparency, accountability, and political will. And we all know how much we love those things.
Until then, keep your spreadsheets. I’ll be here, waiting for the system to collapse under its own weight.
Cara C
December 29, 2025
I just wanted to say thank you for writing this. I’ve been a pharmacist for 18 years and I’ve been drowning in this stuff. I used to dread CE. Now I look forward to it-because I finally found the right courses. The case studies? Game-changer. I actually remember what I learn now.
And the Orange Book? I used to ignore it. Now I check it every Monday. I set a reminder. I keep a little notebook. I even started sharing updates with my team. One of my techs said, ‘I didn’t know we could do this.’ And I said, ‘Yeah. We can. We just never did.’
It’s not about being perfect. It’s about being consistent. Ten minutes a week. That’s it. You don’t need to memorize everything. You just need to know where to look.
And to the people saying this is all a scam? I get it. I’ve been there. But every time I catch a substitution error before it happens-because I checked the TE code-I know this matters. It’s not about the system. It’s about the person holding the bottle. And if we don’t get this right, someone gets hurt.
So I keep checking. I keep learning. I keep caring. Because someone’s life depends on it.
Erika Putri Aldana
December 31, 2025
why do we even care about te codes? no one else does. the patient doesn't care. the doctor doesn't care. the insurance company just wants the cheapest thing. so why are we stressing? just give them the generic. if they have a problem, they'll say something. if not, they're fine. stop making pharmacy so complicated. it's just pills. you don't need a phd to hand them out. just stop overthinking it.
Grace Rehman
January 1, 2026
Generics aren’t the problem. The system is.
We treat pharmacists like technicians, not clinicians. We give them a mountain of rules, a dozen conflicting state laws, and then tell them to be experts on bioequivalence, biosimilars, REMS, and TE codes-all while managing 200 prescriptions a day.
And then we wonder why they burn out.
CE isn’t the answer. Compassion is. Autonomy is. Trust is.
What if we stopped treating pharmacists like potential criminals and started treating them like professionals? What if we trusted them to look up a TE code instead of forcing them to memorize 1,200 of them? What if we gave them time-not more paperwork?
Maybe the real CE is a 15-minute conversation with a colleague. Maybe it’s a quiet moment to pause before dispensing. Maybe it’s knowing you’re not alone in this mess.
We don’t need more courses. We need more humanity.
And if you’re still checking the Orange Book every week? Good for you. But don’t make the rest of us feel guilty for being human.
Jerry Peterson
January 2, 2026
I’m from the Midwest. We don’t have fancy apps or ACPE-certified case studies. We have one pharmacy tech, two pharmacists, and a printer that jams every Tuesday.
But we still check the Orange Book. Not because we’re told to. Because we’ve seen what happens when we don’t.
A 72-year-old woman came in last month with a new prescription for levothyroxine. She’d been on the same brand for 10 years. We switched her to a generic-same TE code. She came back two weeks later dizzy, heart racing. We checked the Orange Book. The manufacturer had changed the formulation. The TE code had been downgraded to BX. We hadn’t known.
That’s why we check.
It’s not about rules. It’s about people. I don’t care if it’s 10 minutes a week. If it keeps someone from ending up in the ER, it’s worth it.
And yeah, the system’s broken. But we’re still here. Still doing the work. Still showing up.
That’s what matters.
Adrian Thompson
January 3, 2026
Let’s be honest-this whole generics thing is just another way for Big Pharma to control the market. The FDA approves generics from companies in China and India that have zero oversight. The bioequivalence standards? A joke. They test on 20 healthy college kids and call it science.
And now they want us to check the Orange Book every week? Like we’re supposed to be the FDA’s unpaid watchdogs? Meanwhile, the same companies that make the generics are the ones lobbying Congress to keep the rules weak.
And don’t get me started on biosimilars. They’re not even real drugs. They’re biological Frankensteins. The FDA doesn’t even know how they work. But we’re supposed to trust them? And then state laws change every year? That’s not regulation. That’s chaos.
And CE courses? They’re all written by the same 3 companies that get paid by Big Pharma. They’re not teaching us. They’re brainwashing us.
Stop checking the Orange Book. Start questioning the system.
Because the real danger isn’t a wrong TE code. It’s blind trust in a broken system.
Orlando Marquez Jr
January 3, 2026
While the intent of this post is commendable, its prescriptive tone risks reinforcing a compliance-centric paradigm that undermines professional autonomy. The emphasis on procedural adherence-checking the Orange Book, completing ACPE modules, maintaining spreadsheets-implicitly reduces the pharmacist’s role to that of an information processor rather than a clinical decision-maker.
True professional development lies not in the accumulation of CE credits, but in the cultivation of clinical reasoning, reflective practice, and interprofessional collaboration. A pharmacist who consults with a prescriber about a TE code change, who engages in patient counseling about bioavailability nuances, who participates in a multidisciplinary medication review-these are the acts of true competence.
While regulatory frameworks are necessary, they should serve as scaffolding, not the foundation. The real challenge is not in tracking TE codes, but in ensuring that pharmacists are empowered, compensated, and trusted to exercise judgment.
Perhaps the most valuable CE is not a course, but a conversation.
Jackie Be
January 5, 2026
OMG I JUST REALIZED I DIDN’T CHECK THE ORANGE BOOK LAST MONTH AND I SWITCHED 3 PEOPLE TO A NEW LEVOTHYROXINE GENERIC AND ONE OF THEM WAS MY MOM AND NOW I’M SCARED SHE’S GOING TO HAVE A HEART ATTACK AND I’M GONNA GET SUED AND I’M GOING TO JAIL AND MY LIFE IS OVER 😭😭😭
Brian Furnell
January 6, 2026
Jackie-calm down. You didn’t kill anyone. You checked the TE code before you dispensed, right? If it was AB, you’re fine. If it changed to BX after you dispensed? That’s on the FDA, not you.
And your mom? She’s fine. She’s not going to have a heart attack from a generic switch. Levothyroxine is tricky, yes-but the body adapts. The real risk is if she’s on multiple brands back-to-back without monitoring.
Go check the Orange Book now. Look up the drug. See the current code. If it’s AB, you’re golden. If it’s BX? Call her doctor. Tell them you’re concerned. That’s what we do. We don’t panic. We act.
You’re not alone. We’ve all been there. You’re a good pharmacist. Breathe.
Christina Weber
January 6, 2026
Jackie, you’re not alone. I’ve been there too. I once switched a patient to a new generic, didn’t check the Orange Book, and two days later the patient came back with a seizure. Turned out the TE code had changed from AB to BX. I didn’t know.
It wasn’t because I was lazy. It was because the system doesn’t give us time. We’re rushing between 150 prescriptions, a refill call, and a patient asking why their blood pressure med tastes weird.
But here’s the thing-you didn’t ignore it. You noticed. You cared. That’s what separates good pharmacists from the rest.
Go check the code. Call the doctor. Update your records. And then-take a breath. You’re not a failure. You’re human.
And you’re not going to jail.
Write a comment