Switching from a brand-name drug to a generic might save you money-but it could also trigger an unexpected reaction. You’re not imagining it. The active ingredient is the same, but the rest of the pill? That’s where things get tricky. Most people don’t realize that up to 99% of a pill can be made of inactive ingredients. These are the fillers, dyes, preservatives, and binders that help the medicine hold its shape, taste better, or last longer. And for some people, they’re not harmless at all.
Why Generics Can Trigger Allergies When Brand Names Don’t
Generic drugs are required by the FDA to have the same active ingredient as the brand version, and they must deliver it the same way. But there’s no rule saying they have to use the same inactive ingredients. That means a 10mg tablet of Singulair® might contain lactose, while the 4mg version doesn’t. The same drug, different fillers. One version could be safe for you; the other could cause a rash, stomach cramps, or even an asthma attack. The problem isn’t rare. A 2019 study from Brigham and Women’s Hospital and MIT looked at over 42,000 oral medications and found that 92.8% of them contained at least one ingredient that could trigger a reaction in sensitive people. Lactose shows up in about 45% of all pills. Food dyes like Red #40 or Yellow #5? Present in 33%. Gluten? Hidden in some. Soy oil? Egg? Gelatin? All common. And most of them aren’t labeled clearly. For someone with a milk allergy, a pill with lactose might cause bloating or diarrhea. For someone with Celiac disease, even trace gluten can damage the gut. And if you’re allergic to sulfites, a preservative used in some medications, you could face wheezing or chest tightness. These aren’t theoretical risks. Pharmacists report that 87% of them have seen patients react after switching from brand to generic-even though the active ingredient hadn’t changed.What Are the Most Common Problematic Ingredients?
Not all inactive ingredients are created equal. Some are harmless for nearly everyone. Others are red flags for specific groups. Here are the most frequent culprits:- Lactose - Found in over 20% of prescription drugs and 6% of over-the-counter meds. A major issue for people with severe milk protein allergy or lactose intolerance.
- Gluten - Used as a binder in some pills. Even small amounts can harm people with Celiac disease. Not all manufacturers disclose it.
- FD&C dyes - Yellow #5, Red #40, Blue #1. Linked to hives, asthma, and hyperactivity in sensitive individuals. Often used for color, not function.
- Bisulfites - Preservatives like sodium metabisulfite. Known to trigger severe asthma reactions. These are one of the few ingredients that must be labeled by the FDA.
- Gelatin - Used in capsules. Comes from animal sources (pig, cow). A problem for vegetarians, vegans, or those with meat allergies.
- Soy oil - Used as a lubricant. Can trigger reactions in people with soy allergy, even in tiny amounts.
- Latex - Sometimes found in packaging or stoppers. Not in the pill itself, but can cause reactions during handling or administration.
Why Labeling Is So Confusing
You’d think if a pill contains something dangerous, it would say so on the label. But that’s not how it works. The FDA only requires manufacturers to list certain allergens-like peanut oil or sulfites. Everything else? Optional. That means a pill could contain gluten, soy, or egg protein, and the label might just say “other inactive ingredients.” Even when ingredients are listed, they’re often buried in tiny print on the patient information leaflet. Many people don’t even open it. And if you switch pharmacies or refill your prescription months later, the formula might have changed without you knowing. A 2021 Safe Medication report warns: “The inactive ingredients may be different between brand and generic versions of the same medication.” The European Union requires full disclosure of all excipients since 2019. The result? A 37% drop in allergic reactions to medication ingredients. In the U.S., no such rule exists. Some companies have voluntarily improved labeling since the 2019 MIT study, but it’s not universal. As of 2023, only 12% of generic medications offer an allergen-free version.
What You Can Do: A Practical Step-by-Step Plan
If you’ve ever had a reaction after starting a new pill-or if you have known food allergies-here’s what to do:- Know your triggers. If you’re allergic to milk, gluten, soy, or eggs, get tested by an allergist. Don’t assume you know all your sensitivities. Some reactions are delayed or subtle.
- Create a personal allergen list. Write down every ingredient you react to. Include not just foods, but also things like food dyes or preservatives. Keep this list updated.
- Ask your pharmacist for the full ingredient list. Pharmacists have access to databases that show every ingredient in every version of a drug. Don’t rely on the bottle label. Ask: “Is this version free of lactose, gluten, and artificial dyes?”
- Compare brand and generic versions. Sometimes, the brand version is actually safer for you. If your insurance allows, request the brand name-even if it costs more. Your health is worth it.
- Check for updated formulations. Medication formulas change. A pill that was safe last year might not be this year. Always double-check when refilling.
- Use the Inactive Ingredient Finder app. Developed by MIT researchers and launched in beta in 2023, this free app lets you search any medication by name and see its full excipient profile. It covers 98% of U.S. medications.
When Your Doctor Doesn’t Know the Answer
Many doctors don’t routinely ask about food allergies when prescribing. They assume if the active ingredient is fine, the rest doesn’t matter. But that’s outdated thinking. The 2019 MIT study authors recommend that clinicians specifically ask: “Do you have any food allergies or intolerances?” If your doctor dismisses your concerns, bring your allergist’s notes. Show them the ingredient list. Point out that the FDA itself acknowledges that inactive ingredients can cause “unusual and sometimes severe allergic reactions.” For patients with Celiac disease, the Celiac Disease Foundation reports that only 15% of commonly prescribed drugs are verified gluten-free-even though 78% of gluten-free certification programs now include medications. That means you’re likely on your own to find safe options.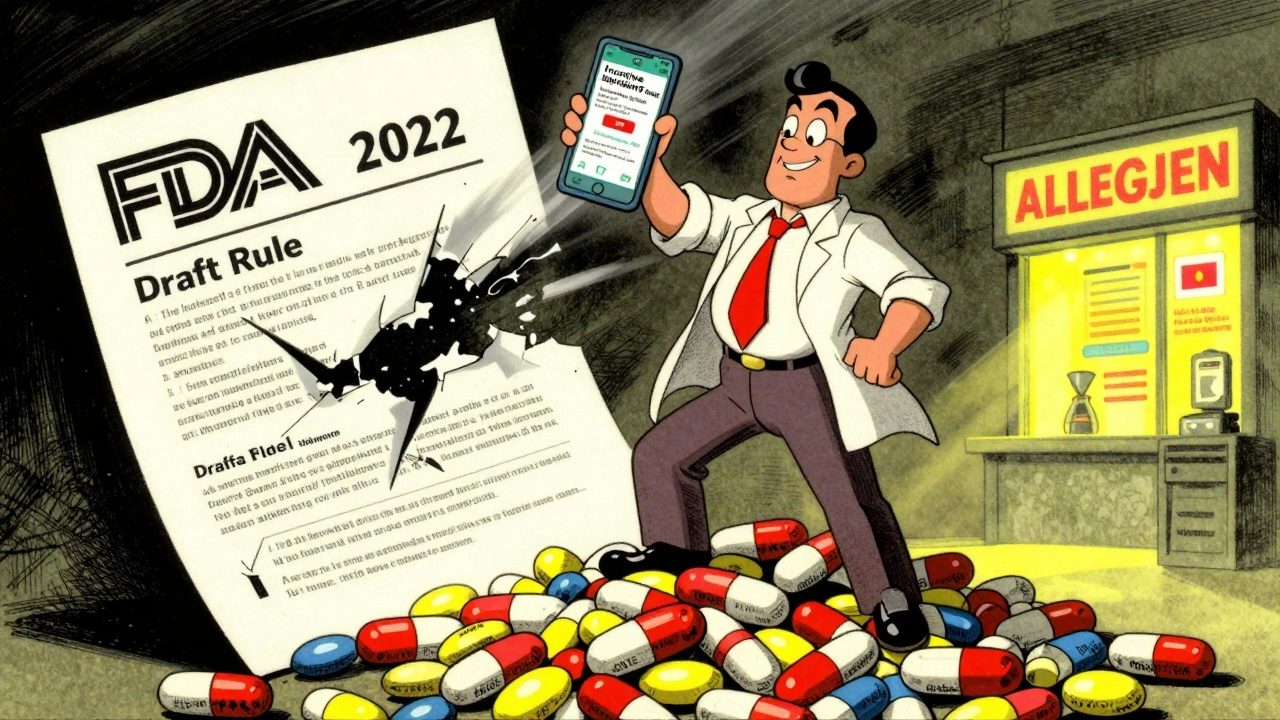
What’s Changing-and What’s Not
There’s progress. The FDA held a public workshop in 2021 on this issue. In 2022, they released draft guidance proposing mandatory labeling for eight high-risk ingredients: lactose, gluten, peanut oil, soy, sulfites, azo dyes, gelatin, and shellfish derivatives. But as of October 2023, it’s still just a draft. No final rule. Meanwhile, pharmacies are slowly upgrading. 42% now use electronic systems that flag potential allergens when filling prescriptions-up from just 17% in 2020. That’s a win. But it’s not enough. The IQVIA Institute predicts that by 2027, 30% of new generic drugs will offer at least one allergen-free version. That’s hopeful. But for now, if you’re sensitive, you need to be your own advocate.Final Thought: You’re Not Overreacting
It’s easy to feel like you’re being too picky. “It’s just a pill. How bad could it be?” But for people with true allergies, it’s not about being difficult-it’s about staying safe. A reaction to an inactive ingredient isn’t a myth. It’s a documented medical reality. If you’ve had a reaction after switching meds, you’re not alone. And you’re not wrong. The system isn’t built to protect you yet. But you can protect yourself-with knowledge, questions, and the right tools. Keep asking. Keep checking. Keep demanding clarity. Your body deserves nothing less.Can generic drugs cause allergic reactions even if the active ingredient is the same?
Yes. Generic drugs must match the active ingredient of the brand version, but they can use different inactive ingredients like lactose, gluten, dyes, or preservatives. These can trigger allergic reactions or intolerances in sensitive individuals, even when the therapeutic effect is identical.
How do I find out what’s in my medication?
Check the patient information leaflet that comes with your prescription. If it’s not clear, ask your pharmacist for the full inactive ingredient list. Many pharmacies use digital tools that show excipient details. You can also search your drug in the free MIT-developed Inactive Ingredient Finder app, which covers 98% of U.S. medications.
Is lactose in pills a problem for people with milk allergy?
Yes. Lactose is used in over 20% of prescription drugs. While it’s not the same as milk protein, some people with severe milk allergies react to lactose due to cross-contamination or immune sensitivity. Pediatric patients are especially at risk. Always confirm with your allergist if lactose is safe for you.
Are there any medications that are guaranteed to be gluten-free?
Very few. Only about 15% of commonly prescribed drugs are verified gluten-free by certification programs. The FDA doesn’t require gluten labeling, so you can’t assume a drug is safe. Always check with your pharmacist or use the Inactive Ingredient Finder app to verify.
Why don’t drug companies use the same inactive ingredients in generics and brands?
Cost and availability. Generic manufacturers choose cheaper, more accessible fillers. A brand might use a high-purity lactose, while the generic uses a lower-grade version that still meets FDA standards. There’s no requirement to match the brand’s excipients-only the active ingredient’s performance.
Can I request a brand-name drug instead of a generic if I have allergies?
Yes. If your doctor writes “Do Not Substitute” or “Brand Necessary” on the prescription, your pharmacy must fill it with the brand name. Insurance may require prior authorization, but if you have documented allergies or reactions, your request is medically valid and often approved.
Are there any new developments to make medications safer for allergy sufferers?
Yes. The FDA has proposed new labeling rules for eight high-risk ingredients, though they’re not finalized yet. Pharmacies are adopting allergen-filtering software, and over 68% of major drugmakers have improved labeling voluntarily since 2019. By 2027, experts predict 30% of new generics will offer at least one allergen-free version.





Comments
Chelsea Moore
December 3, 2025
I can't believe this is even a thing!!! Seriously?? We're putting LACTOSE in pills?? And gluten?? And DYES?? This isn't medicine-it's a chemical roulette game!! And the FDA just sits there like a bored librarian?? I had a full-blown anaphylactic reaction to a generic ibuprofen because of Red #40-and they told me I was 'overreacting'!! I'm not overreacting-I'm surviving!! Someone needs to sue these companies!!
Fern Marder
December 3, 2025
OMG YES!! 🙌 I’ve been saying this for YEARS!! My kid got hives from a generic Adderall because of Yellow #5. The pharmacist didn’t even know to check. Now I print out the ingredient list for every single script. I keep a folder. I’m basically a pharmaceutical detective now. 🕵️♀️💊 #MedicationAllergiesAreReal
Anthony Breakspear
December 3, 2025
Look, I get it-people are scared. But let’s not turn this into a panic. The system’s broken, sure. But the solution isn’t to freak out-it’s to get smart. Ask your pharmacist. Use the MIT app. Know your triggers. I used to be one of those people who just swallowed whatever was handed to me. Then my wife had a reaction to gelatin capsules. Now? We check everything. It’s not hard. It just takes 2 minutes. You don’t need a conspiracy-you need a checklist.
Sandi Allen
December 5, 2025
They're hiding it on purpose!! Lactose? Gluten? Soy? It's all a BIG PHARMA scam!! They know people with allergies are vulnerable-and they're using it to make more money!! Why else would they NOT label it? Because if you knew what was really in there, you'd refuse!! They're poisoning us slowly!! I checked my blood after switching generics-my IgE levels spiked!! This is bioweapon territory!!
John Webber
December 5, 2025
so like… if you allergic to milk you cant take any pills? what about the ones with lactose? do you just not take meds? i mean its just a little bit right? like a speck? i think people make it into a bigger deal than it is
Shubham Pandey
December 6, 2025
Generic drugs are fine. Stop overthinking.
Elizabeth Farrell
December 6, 2025
I just want to say how much this article meant to me. For years, I thought I was being dramatic when I’d get stomach cramps after switching pills. I’d blame myself-'Maybe I ate something bad,' or 'I’m just anxious.' But no. It was the lactose. Or the dye. Or the gelatin. I finally asked my pharmacist for the full list, and it was like a light switched on. I’m not broken. The system is. And now I’m learning how to navigate it. To anyone else feeling alone in this-you’re not. We’re all just trying to survive a system that doesn’t care enough to label things properly. Thank you for writing this. I’m sharing it with my whole family.
Sheryl Lynn
December 7, 2025
How quaint. You’re all treating this like some novel revelation. In Europe, this has been standard since 2019. We have *transparency*. Here? We have a pharmaceutical-industrial complex that treats patients like disposable test subjects. And yet, you’re all shocked? Darling, this isn’t negligence-it’s capitalism with a pill-shaped logo. If you’re not using the MIT app, you’re not just uninformed-you’re complicit. And if you think a pharmacist knows more than the label? Honey, they’re just the middleman with a clipboard.
Paul Santos
December 8, 2025
It’s a classic case of epistemic asymmetry in pharmaceutical regulation, isn’t it? The active ingredient is the ontological core-yet the excipients are the phenomenological variables that determine lived experience. We’ve reduced medicine to a functionalist paradigm, ignoring the hermeneutics of bodily response. The FDA’s draft guidance? A token gesture. What we need is a hermeneutic framework for excipient literacy. Until then, we’re all just guessing in the dark… with our immune systems.
;-)
John Biesecker
December 9, 2025
i never thought about this but wow. my grandma takes 7 pills a day and she gets bloated every time they switch generics. she just says 'oh i'm getting old' but now i think it's the lactose. i'm gonna print this out and show her. thanks for the app too, i just downloaded it. 🙏
Genesis Rubi
December 10, 2025
Why are we letting foreign companies make our meds? This is why America is falling apart. We used to make everything here. Now we import pills with soy and gluten from China and India and then wonder why people are sick? Wake up. Buy American. Or don't complain when your body rebels.
Doug Hawk
December 11, 2025
Just want to add something-my allergist told me to always ask for the 'lot number' when you pick up a prescription. That way, you can call the manufacturer and get the exact excipient breakdown for that batch. Most people don't know this. It's not in the article, but it's gold. I've caught 3 formulation changes this way. You're not paranoid if you're prepared. And yes, the MIT app is legit. I use it daily.
Write a comment