Every year, thousands of people end up in the hospital not because their condition got worse, but because two medications they were taking started fighting each other. This isn’t rare. It’s common. And it’s preventable. Drug-drug interactions (DDIs) happen when one medicine changes how another works in your body-sometimes making it stronger, weaker, or even dangerous. Understanding how these interactions work isn’t just for doctors. If you’re taking more than one medication, you need to know the basics.
What Exactly Is a Drug-Drug Interaction?
A drug-drug interaction occurs when one medication affects the way another medication behaves in your body. It’s not about side effects from a single drug. It’s about the combination. Two drugs that are safe on their own can become risky together.
There are two main types: pharmacokinetic and pharmacodynamic. One is about what your body does to the drugs. The other is about what the drugs do to each other.
Pharmacokinetic Interactions: How Your Body Moves the Drugs
This is the most common type of interaction. It’s all about absorption, distribution, metabolism, and excretion-basically, how your body gets the drug in, moves it around, breaks it down, and gets it out.
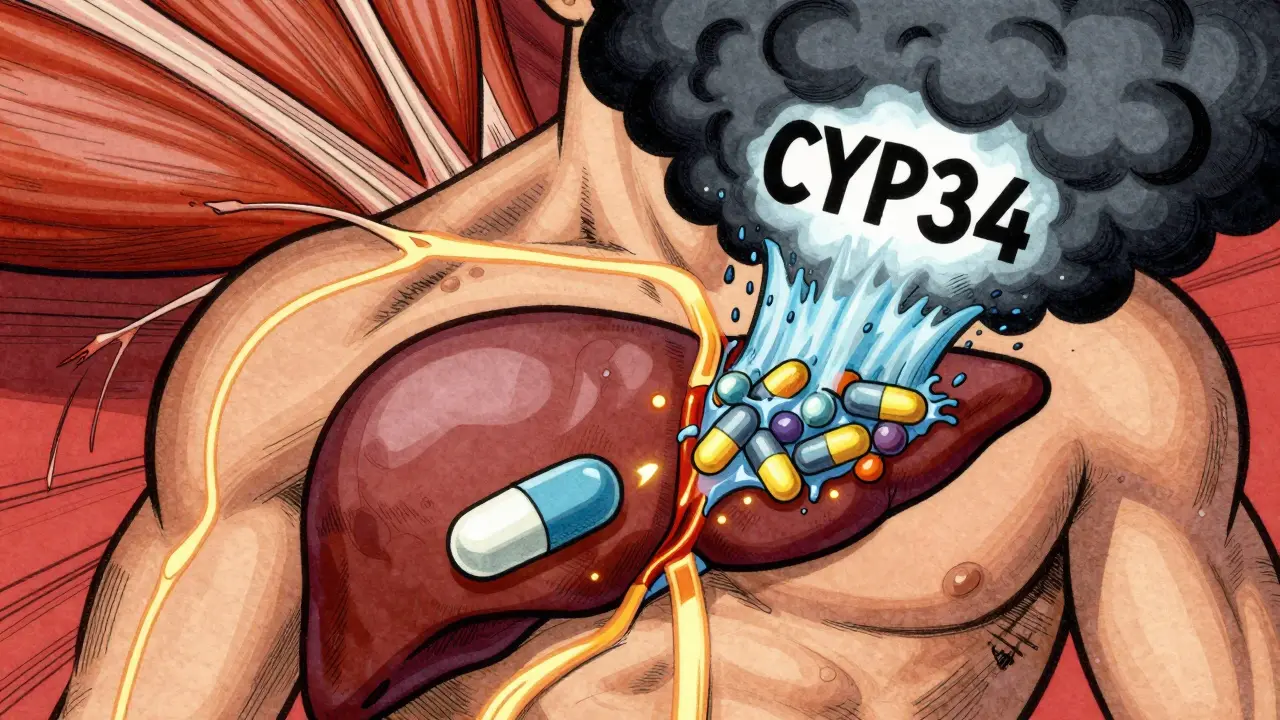
Let’s say you take a statin like simvastatin to lower cholesterol. Now you add ketoconazole, an antifungal. Ketoconazole blocks an enzyme in your liver called CYP3A4, which normally breaks down simvastatin. Without that enzyme doing its job, simvastatin builds up in your blood-by 10 to 20 times. That’s not just a small increase. That’s enough to cause rhabdomyolysis, a serious muscle breakdown that can lead to kidney failure.
CYP3A4 is responsible for breaking down about half of all prescription drugs. Other key enzymes include CYP2D6, CYP2C9, and CYP2C19. If a drug inhibits (blocks) one of these, it can cause other drugs to pile up. If it induces (speeds up) the enzyme, it can make other drugs disappear too fast.
Take St. John’s Wort, a popular herbal supplement for mood. It’s a strong inducer of CYP3A4. If you’re on cyclosporine (an immune suppressant after a transplant), St. John’s Wort can slash cyclosporine levels by 50-60%. That means your body might reject the new organ.
It’s not just enzymes. Transporters matter too. P-glycoprotein (P-gp) is like a bouncer at the cell door-it kicks drugs out of cells. If you take verapamil (a blood pressure drug), it blocks P-gp. That means digoxin (used for heart rhythm) can’t get kicked out. Digoxin builds up. Too much can cause deadly heart rhythms.
Pharmacodynamic Interactions: When Drugs Talk to Each Other
This is less about chemistry and more about biology. Two drugs hit the same target in your body and either amplify or cancel each other out.
Think of it like two people pulling on a rope. If they pull in the same direction, the rope moves faster. If they pull opposite ways, nothing happens-or worse, the rope snaps.
One classic example: fluoroquinolone antibiotics (like ciprofloxacin) combined with macrolides (like erythromycin). Both can prolong the QT interval on an ECG. Alone, the risk is low. Together, the chance of torsades de pointes-a life-threatening heart rhythm-goes up by 5.7 times.
Another: ACE inhibitors (like lisinopril) plus potassium-sparing diuretics (like amiloride). Both raise potassium levels. Together, they can push serum potassium up by 1.0-1.5 mmol/L. That’s enough to cause cardiac arrest.
And then there’s the opposite: antagonism. If you take an opioid painkiller and a benzodiazepine (like diazepam) for anxiety, both depress your breathing. Together, they can slow it to a dangerous level. That’s why the CDC warns against combining them.
Who’s at Risk?
Anyone taking multiple medications is at risk. But some groups are hit harder.
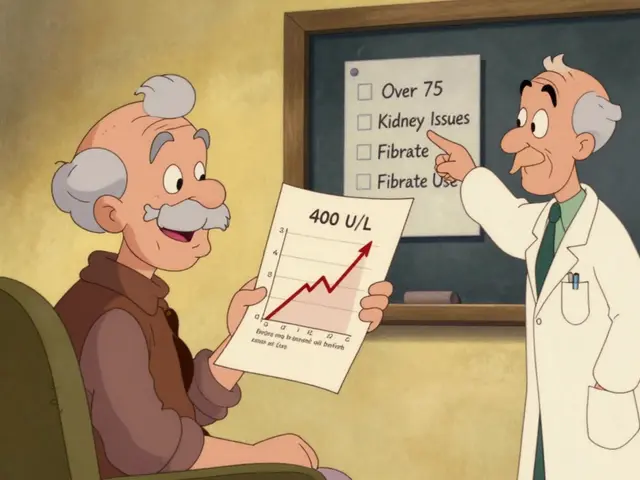
People over 65 are the most vulnerable. On average, they take 4-5 prescription drugs daily. The Beers Criteria, updated in 2019, lists 30 high-risk combinations for older adults. One of the worst? NSAIDs (like ibuprofen) with blood thinners like warfarin. That combo triples or quadruples the risk of major bleeding.
People with chronic conditions-heart disease, diabetes, HIV-are also at higher risk because they’re often on multiple long-term meds. In HIV care, the Liverpool HIV-Drug Interactions Checker is used daily by clinicians to screen over 350 antiretroviral combinations. That’s how complex it can get.
Genetics play a role too. Some people are poor metabolizers of CYP2D6. Codeine, a painkiller, needs CYP2D6 to turn into morphine. If you’re a poor metabolizer, codeine doesn’t work. If you’re an ultrarapid metabolizer, you turn it into morphine too fast. Add a CYP3A4 inhibitor like clarithromycin, and you risk morphine overdose-even with normal doses.
How Are These Interactions Found?
Drug companies test for interactions before a drug hits the market. They start in labs: human liver cells, enzyme cultures, transporter assays. If a drug looks like it might block CYP3A4, they move to clinical trials with healthy volunteers.
The FDA and EMA have clear rules. If a drug has a [I]/Ki ratio ≥0.1 for CYP inhibition, a clinical study is required. If it’s a substrate of OATP1B1 and the [I]2/[IC50] ratio is ≥0.1, they must test transporter interactions too.
But real-world data is where the real picture shows up. The FDA’s FAERS database tracked over 12,800 DDI-related reports between 2010 and 2020. Warfarin was in nearly 30% of them. Antidepressants? 15%. Anticoagulants? 12%. These aren’t edge cases. They’re the norm.
What Happens When It Goes Wrong?
DDIs don’t just cause side effects. They cost money. A 2019 study estimated preventable drug interactions cost the U.S. healthcare system $1.3 billion a year. Most of that comes from hospital stays-bleeding from warfarin interactions, muscle damage from statins, kidney failure from NSAIDs.
And it’s not just hospitals. Emergency rooms, nursing homes, and clinics all see the fallout. In elderly patients, DDIs account for 3-5% of all hospital admissions. That’s tens of thousands of people every year who didn’t need to be there.
How Do We Prevent Them?
There’s no magic bullet, but there are proven strategies.
First, pharmacists. A 2021 study showed pharmacist-led reviews reduced serious DDIs by 37% in over 12,500 patients. They check every prescription, spot hidden risks, and talk to doctors.
Second, electronic health records. Most now have DDI alerts. But here’s the problem: 80-90% of those alerts are false. Clinicians get tired of being told everything is dangerous. So they ignore them. That’s called alert fatigue. Newer systems like Epic’s ‘Suggestive Warnings’ use context-patient age, kidney function, current meds-to cut down noise. One study showed they cut high-severity DDIs by 22%.
Third, patient education. If you’re on warfarin, your doctor should tell you about vitamin K-rich foods (kale, spinach, broccoli). Too much vitamin K makes warfarin less effective. Too little? Risk of clotting. It’s a tight balance.
And don’t forget supplements. People think ‘natural’ means safe. But St. John’s Wort, garlic, ginkgo, and even grapefruit juice can cause serious interactions. Grapefruit juice blocks CYP3A4. One glass can change how your body handles a whole class of drugs.
The Future: Personalized Medicine and AI
The next big leap is personalization. Pharmacogenomics looks at your genes to predict how you’ll respond to drugs. CPIC has published 22 guidelines on this. If you’re a CYP2D6 ultrarapid metabolizer, you shouldn’t take codeine at all-especially if you’re also on a CYP3A4 inhibitor.
And AI is catching up. A 2021 study trained a machine learning model on 89 million electronic health records. It predicted DDIs with 94.8% accuracy-far better than old rule-based systems. It doesn’t just look at two drugs. It looks at your age, liver function, other meds, even your diagnosis. That’s the future.
NIH is pouring $14.7 million into DDI research in 2022 alone. They’re studying how gut bacteria affect drug metabolism, how time-dependent enzyme inhibition works, and how to better predict transporter interactions.
What You Can Do Today
You don’t need to be a scientist to protect yourself.
- Keep a list of everything you take: prescriptions, over-the-counter meds, vitamins, supplements, herbs.
- Bring that list to every doctor visit-even if you think it’s not important.
- Ask your pharmacist: ‘Could any of these interact?’ Don’t wait for them to ask you.
- If you start a new medication, ask: ‘What should I watch out for?’
- Don’t stop or change doses without talking to your provider.
Drug interactions aren’t mysterious. They’re predictable. And they’re preventable-with awareness, communication, and a little caution.
What are the most dangerous drug-drug interactions?
Some of the most dangerous combinations include warfarin with NSAIDs (increased bleeding risk), statins with strong CYP3A4 inhibitors like ketoconazole (risk of rhabdomyolysis), and ACE inhibitors with potassium-sparing diuretics (dangerous hyperkalemia). Combining benzodiazepines with opioids can cause fatal respiratory depression, and fluoroquinolones with macrolides can trigger life-threatening heart rhythms. These aren’t rare-they’re well-documented and often preventable.
Can over-the-counter drugs cause interactions?
Absolutely. Common OTC drugs like ibuprofen, naproxen, and even antacids can interact. Ibuprofen increases bleeding risk when taken with warfarin or aspirin. Antacids can reduce absorption of antibiotics like ciprofloxacin. Even herbal supplements like St. John’s Wort, garlic, and ginkgo can interfere with prescription meds. Just because something is sold without a prescription doesn’t mean it’s safe to mix.
How do I know if a drug is a CYP3A4 substrate?
Common CYP3A4 substrates include simvastatin, atorvastatin, cyclosporine, tacrolimus, sildenafil, midazolam, and many HIV medications. If you’re taking one of these and start a new drug-especially an antifungal, antibiotic, or seizure med-ask your pharmacist or doctor if it affects CYP3A4. The drug label often says so under ‘Drug Interactions.’
Do grapefruit juice and alcohol cause drug interactions?
Yes. Grapefruit juice blocks CYP3A4 in the gut, which can increase blood levels of many drugs-sometimes to dangerous levels. Even one glass can have an effect for 24 hours. Alcohol doesn’t directly inhibit enzymes like grapefruit, but it can worsen sedation with benzodiazepines or increase liver damage with acetaminophen. It also raises the risk of bleeding with anticoagulants.
Why do some people have worse interactions than others?
Genetics, age, liver and kidney function, and even gut bacteria play a role. For example, CYP2D6 poor metabolizers process certain drugs much slower, making them more sensitive to interactions. Older adults have slower metabolism and often take more drugs. People with liver disease can’t break down drugs as well. All of this makes some people far more vulnerable than others.



Comments
Kenji Gaerlan
January 22, 2026
man i just take my pills and hope for the best. why do i gotta learn all this enzyme crap? my grandma takes 12 things and still walks the dog every morning. maybe we just need less meds and more naps.
Write a comment