When you swallow a pill, you might think it just goes straight to work. But what you eat-or when you eat it-can make that pill work better, worse, or not at all. It’s not magic. It’s science. And it’s happening every time you take medicine with breakfast, lunch, or dinner.
Why Food Changes How Medicines Work
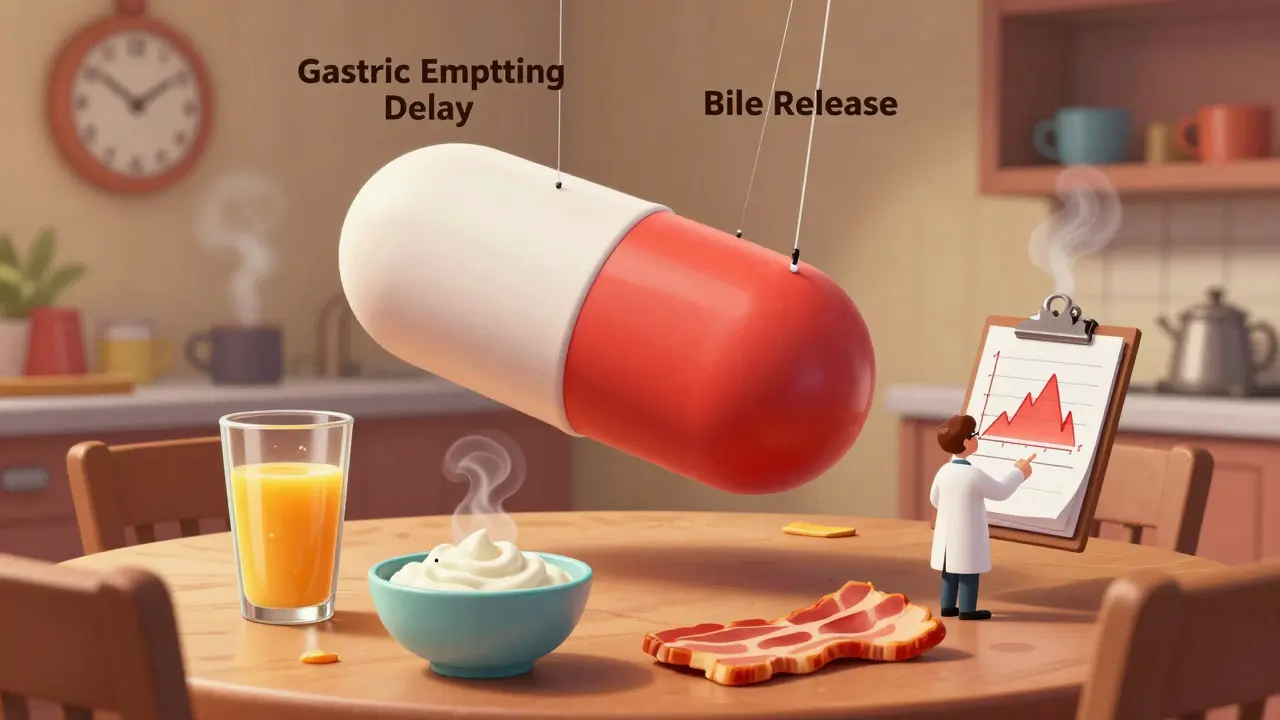
Food doesn’t just fill your stomach. It changes how your body handles medicine. When you eat, your stomach slows down. Gastric emptying-the process of moving food and pills into the small intestine-can drop by 30% to 50%. That means your pill sits in your stomach longer before it starts being absorbed. For some drugs, that delay doesn’t matter. For others, it can mean the difference between healing and hospitalization. Fats play a big role. A high-fat meal-think bacon, cheese, fried food-can hold up stomach emptying for 1.5 to 2 extra hours. That’s why drugs like griseofulvin (an antifungal) absorb up to 300% better with food. The fat triggers bile release, which helps dissolve the drug so your body can grab it. But for drugs that need acid to dissolve-like itraconazole, used for fungal infections-high-fat meals raise stomach pH, making absorption drop by 40%. Calcium is another troublemaker. Dairy products, fortified orange juice, even some antacids can bind to antibiotics like tetracycline and doxycycline. That binding blocks absorption. Studies show up to 75% less drug gets into your bloodstream if you take these antibiotics with milk or yogurt. The result? A treatment that doesn’t work-and a lingering infection.Empty Stomach: What It Really Means
When your doctor says “take on an empty stomach,” they don’t mean “don’t eat for a week.” They mean: one hour before or two hours after eating. That’s the window your stomach needs to clear out so the drug can move freely into the small intestine. Levothyroxine, the thyroid hormone replacement, is the classic example. Food can reduce its absorption by 30% to 55%. That’s not a small drop. It’s enough to leave you tired, cold, and gaining weight-even if you’re taking the right dose. Mount Elizabeth Hospital’s 2022 guidelines say the best time is first thing in the morning, with a full glass of plain water, at least 30 minutes before your first bite. Skip the coffee, the toast, the yogurt. Wait. Semaglutide, the weight-loss and diabetes drug, follows the same rule. Taking it within 30 minutes of eating cuts absorption by 44%. That’s why Novo Nordisk’s clinical trials show patients who waited 30+ minutes before meals had better blood sugar control.Take With Food: When Eating Helps
Not all drugs hate food. Some need it. Nitrofurantoin, an antibiotic for urinary tract infections, absorbs 40% better when taken with food. Same with cefpodoxime, another antibiotic. The food doesn’t just help absorption-it reduces stomach upset. For drugs like these, a light snack or even a few crackers can make a big difference. NSAIDs like ibuprofen and naproxen are another case. Taking them on an empty stomach increases your risk of stomach bleeding and acid reflux. A 2022 study found that 42% of users had stomach pain when taking ibuprofen without food. With food? That number dropped to 12%. MyDr.com.au recommends taking them with or right after a meal-not because it helps absorption, but because it protects your gut. Even some diabetes pills need food. Sulfonylureas like glipizide trigger insulin release. If you take them without eating, your blood sugar can crash below 70 mg/dL. That’s dangerous. Symptoms: shaking, sweating, confusion, even passing out. The American Diabetes Association reports 23% of patients on these drugs experience hypoglycemia because they took them on an empty stomach.Timing Isn’t Just About Meals-It’s About Routine
The biggest mistake people make isn’t eating the wrong thing. It’s being inconsistent. A 2023 review in Australian Prescriber found that for most chronic medications, the exact timing doesn’t matter as long as you do it the same way every day. If you take your blood pressure pill with dinner, stick with dinner. If you take your cholesterol drug with breakfast, keep doing it. Consistency matters more than perfection. But for the 25% of drugs that are sensitive to food-like levothyroxine, certain antibiotics, or diabetes meds-timing is critical. That’s where phone alarms help. Set one for 60 minutes before breakfast if you’re on levothyroxine. Set another for 30 minutes after dinner if you’re on glipizide. Apps like Medisafe and MyTherapy now include food-timing reminders. Users who turn them on reduce timing errors by 27%.What About Special Diets?
The old rule was “take with a high-fat meal” for testing. But diets have changed. Gluten-free, plant-based, low-carb-these aren’t trends anymore. They’re normal. The FDA’s 2023 draft guidance now requires food-effect studies to include plant-based meals and low-fat options. That’s because a vegan taking a drug with tofu and rice might absorb it differently than someone eating steak and fries. A 2023 study in Lancet Digital Health showed that personalizing levothyroxine timing based on individual gastric emptying rates improved outcomes by 22%. That’s the future: not one-size-fits-all, but personalized timing.Who’s at Risk?
You’re more likely to have a food-drug interaction if you:- Take five or more medications (polypharmacy)
- Are over 65
- Have trouble remembering doses
- Use multiple pharmacies
- Take supplements or herbal products

Real Stories, Real Consequences
On Reddit, a user named u/ThyroidWarrior shared how their recurring UTI didn’t clear up-until they stopped taking doxycycline with their morning yogurt. Two hours apart? The infection vanished. On Drugs.com, 62% of 1,247 users taking levothyroxine said they struggled with the empty-stomach rule. Many thought “no food” meant “no coffee.” But coffee, even black, can interfere. So can calcium supplements, iron pills, and soy milk. One woman took her pill at 7 a.m., then had oatmeal with almond milk at 7:15. Her TSH levels stayed high for months. Only when she moved her pill to 6 a.m. and waited until 7:30 to eat did she feel normal again.What Should You Do?
Here’s your simple checklist:- Check the label. Look for “take on empty stomach,” “take with food,” or “take with a meal.”
- Ask your pharmacist. They know the details. Don’t assume “with food” means a full meal. Sometimes a banana or a handful of nuts is enough.
- Set a reminder. Use your phone or a pill app. Timing errors are the #1 reason treatment fails.
- Be consistent. If you take your pill with breakfast, always take it with breakfast.
- Separate calcium and antibiotics. Wait two hours between dairy and tetracycline, doxycycline, or ciprofloxacin.
- Don’t skip meals. If your medicine needs food, don’t skip breakfast just to “follow instructions.” Have a small snack.
What’s Next?
The future of medication timing is smarter. Ingestible sensors that track stomach pH and emptying are already in trials. Imagine a pill that sends a signal to your phone: “Your stomach is ready.” That’s not sci-fi-it’s coming. For now, the best tool you have is knowledge. Food isn’t the enemy. It’s part of the equation. Get the timing right, and your medicine works like it should. Get it wrong, and you’re paying for a drug that doesn’t work.Can I take my medication with coffee?
It depends on the drug. Coffee can interfere with thyroid medication (like levothyroxine), some antibiotics, and certain antidepressants. For most other pills, black coffee is usually fine-but wait at least 30 minutes after taking the medicine. If you’re unsure, check with your pharmacist.
What if I forget and take my pill with food?
If you’re on a drug that needs an empty stomach-like levothyroxine or certain antibiotics-don’t panic. Just wait until your next scheduled dose and go back to the correct timing. Don’t double up. If you’re on a drug that needs food-like NSAIDs or nitrofurantoin-and you took it on an empty stomach, you might feel more stomach upset, but it’s unlikely to cause harm. Just take the next dose with food.
Does it matter if I take my pill with a snack vs. a full meal?
For some drugs, yes. If the label says “take with food,” a small snack (200-300 calories) is often enough to help absorption or reduce side effects. For example, some HIV meds work fine with a banana or crackers. But for drugs that need fat to dissolve-like griseofulvin or itraconazole-a high-fat meal is required. Always follow the specific instructions on your label or from your pharmacist.
Why do some pills say “take with food” and others say “take on an empty stomach”?
It’s all about how the drug is absorbed. Drugs that dissolve in acid need an empty stomach to stay in the acidic environment of the stomach. Drugs that need fat to dissolve need food to trigger bile release. Drugs that irritate the stomach need food to act as a buffer. The label is based on clinical studies that tested absorption under both conditions.
Can I take my vitamins with my medications?
Not always. Calcium, iron, magnesium, and zinc can block absorption of antibiotics like tetracycline and thyroid meds. Take vitamins at least two hours apart from these drugs. Multivitamins with iron or calcium should be taken separately from your main medications unless your doctor says otherwise.
Medication timing isn’t just about following rules. It’s about making sure your body gets what it needs to heal. Get it right, and you’re not just taking pills-you’re getting results.




Comments
Praseetha Pn
January 19, 2026
Let me tell you something the FDA doesn't want you to know-pharma companies design these food-interaction rules to keep you dependent. They know if you take your meds right, you might actually get better. But if you're confused? You keep buying. I've seen people on levothyroxine for years with TSH levels sky-high, all because their doctor never told them almond milk is just soy milk in disguise. And coffee? Don't even get me started. That stuff's laced with glyphosate anyway. You think it's just caffeine? Nah. It's a chemical weapon against thyroid function. I stopped taking mine with water and switched to filtered rainwater. My energy? Night and day.
Stacey Marsengill
January 20, 2026
Wow. Just wow. You people actually believe this? I've been on 7 meds since I was 42 and I've never once followed any of these 'rules.' I take my antibiotics with pizza, my thyroid pill with my morning latte, and my ibuprofen on an empty stomach because I'm not some fragile flower. Guess what? I'm still alive. And I'm not fat. And I don't feel like a zombie. You're all just scared of your own shadows. Next you'll be telling me to avoid oxygen because it 'interferes' with my blood pressure meds.
Max Sinclair
January 20, 2026
This is actually one of the clearest, most well-researched explainers I've seen on this topic. The breakdown of how fats affect bile release and gastric emptying is spot-on. I work in pharmacy and I see patients mess this up daily-especially with doxycycline and dairy. One guy took his antibiotic with a protein shake full of calcium caseinate and wondered why his UTI came back worse. The part about consistency over perfection is gold. If you take your statin with dinner every night, that’s better than trying to time it perfectly but forgetting half the time. Also, props for mentioning the FDA’s new guidance on plant-based meals. That’s a huge step forward. We need more studies on how vegan diets interact with meds-especially with things like statins and SSRIs.
Dayanara Villafuerte
January 22, 2026
Okay but can we talk about how the real MVP here is the person who set a phone alarm for their levothyroxine? 🙌 I used to be the woman who took it at 7 a.m. then ate oatmeal with almond milk at 7:15. I was tired all the time. Then I downloaded MyTherapy, set a 6 a.m. alarm, and waited until 7:30 to eat. I swear to god, I started seeing colors again. Like, actual colors. Not the grayish haze I’d been living in. Also, coffee? Still drink it. Just not until 8 a.m. 🫖✨ #MedicationWin
rachel bellet
January 22, 2026
The entire premise of this post is a neoliberal pharmacological construct designed to pathologize non-compliance while absolving the medical-industrial complex of responsibility for polypharmacy. The 27% reduction in timing errors via apps? That’s a metric engineered by Big Pharma to sell subscription services. The real issue is that 65% of patients on five or more meds are being prescribed by physicians who don’t even understand pharmacokinetics-let alone gastric emptying dynamics. You’re not failing because you forgot your alarm. You’re failing because your care is fragmented, underfunded, and commodified. The solution isn’t a reminder app-it’s universal healthcare with clinical pharmacists embedded in primary care teams. Until then, you’re just being manipulated into performing compliance.
Robert Davis
January 23, 2026
Interesting. I’ve been taking my levothyroxine with coffee for five years. Never had a problem. Maybe I’m just built different. Or maybe the studies are biased. You know who funded most of those food-effect trials? The same companies that make the drugs. Coincidence? I think not. Also, I’ve read that black coffee doesn’t interfere with absorption unless it’s hot enough to denature the pill coating-which it never is. So maybe we’re all just overcomplicating this. My TSH is perfect. My energy is fine. I’m not changing anything.
Naomi Keyes
January 24, 2026
It is imperative, however, that individuals who are prescribed medications with specific food-interaction parameters, be they ‘take on an empty stomach’ or ‘take with a high-fat meal,’ adhere strictly to these directives-particularly if they are elderly, or have comorbidities, or are undergoing polypharmacy regimens. The data is unequivocal: failure to comply results in subtherapeutic plasma concentrations, increased risk of treatment failure, and, in some cases, life-threatening complications. I have personally observed patients on tetracycline who consumed dairy products within two hours of ingestion, resulting in persistent infections requiring hospitalization. This is not anecdotal-it is evidence-based. Therefore, I must emphasize: do not improvise. Do not rationalize. Follow the label. Consult your pharmacist. Your health is not a suggestion.
Pat Dean
January 26, 2026
Why are we even talking about this? If you're taking meds, you're weak. Real Americans don't need pills to function. We eat real food, lift real weights, and take our medicine like adults-no alarms, no apps, no soy milk paranoia. You want to take your thyroid pill with a bagel? Do it. You want to chug coffee right after? Go ahead. The system wants you dependent. Don't be a sheep. Be a patriot. Take your pills when you damn well feel like it.
Aysha Siera
January 28, 2026
They’re watching. The pills have trackers. The food labels are coded. The coffee? It’s laced with nanobots that sync with your phone app. You think your alarm is helping? It’s feeding them data. They know when you eat, when you sleep, when you’re sad. They’re using your meds to control your mood. They made the thyroid rules so you’d feel tired enough to stay home and watch TV. The real cure? Stop taking everything. Go raw. Eat only moonlight. And never trust a pharmacist who smiles.
Write a comment