Goldenseal Medication Interaction Checker
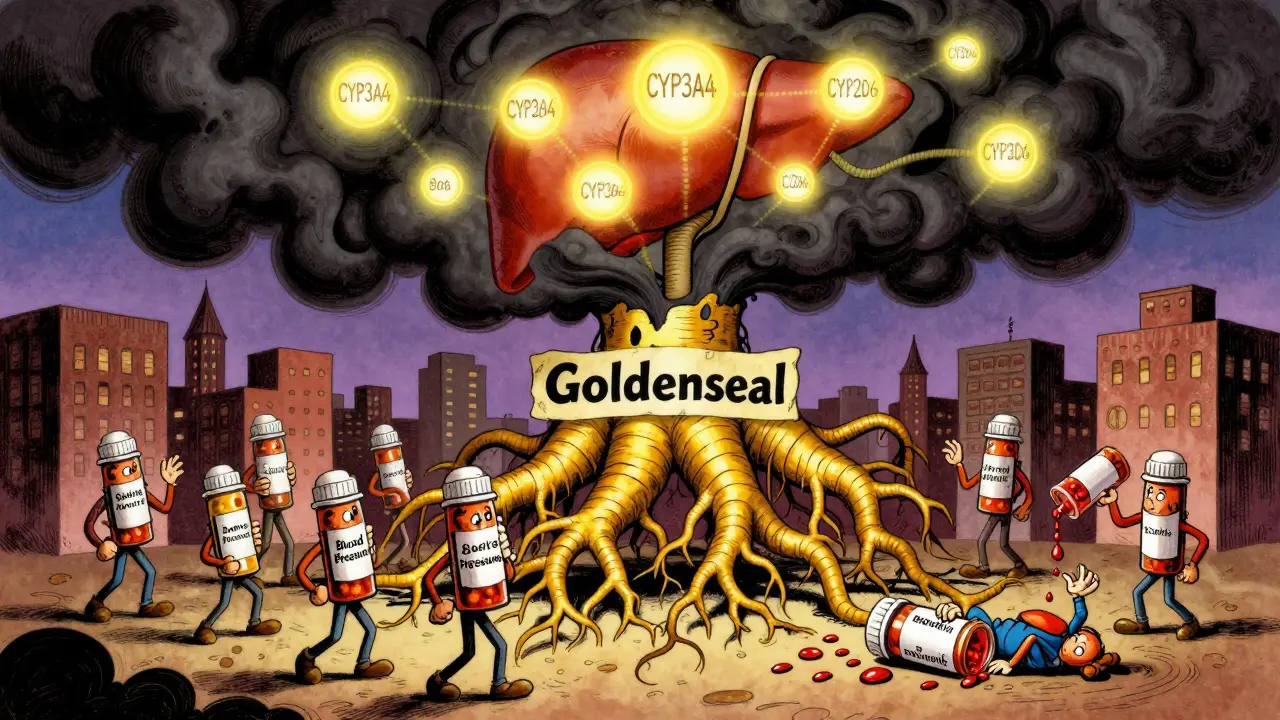
Enter your current medications to check for potential interactions with goldenseal. Goldenseal inhibits liver enzymes (CYP3A4, CYP2D6, etc.) that process many prescription drugs.
Important: This tool provides general information only. Always consult your healthcare provider or pharmacist for personalized advice.
Many people turn to goldenseal for colds, sinus infections, or immune support. It’s marketed as a natural remedy, often sold in capsules, teas, or liquid extracts. But if you’re taking any prescription medication, goldenseal could be hiding a serious risk-liver enzyme interactions that can turn safe drugs into dangerous ones.
What Goldenseal Actually Does in Your Body
Goldenseal comes from the root of a North American herb called Hydrastis canadensis. Its main active ingredients are berberine and hydrastine. These compounds don’t just sit there-they actively interfere with how your liver processes medications. Specifically, they block enzymes called cytochrome P450 (CYP), which are responsible for breaking down about 75% of all prescription drugs.
It’s not just one enzyme. Goldenseal hits five major ones: CYP3A4 (which handles half of all medications), CYP2D6 (responsible for 30%), CYP2C9, CYP1A2, and CYP2E1. That’s unusually broad. Most herbs affect one or two. Goldenseal shuts down a whole system.
For example, if you take a statin like simvastatin, your liver uses CYP3A4 to break it down. If goldenseal blocks that enzyme, the statin builds up in your blood. Too much can cause muscle damage, kidney failure, or worse. Same with blood pressure meds like metoprolol (CYP2D6) or antidepressants like fluoxetine. Their levels can spike 40-60%, leading to dizziness, slow heart rate, or even fainting.
Why This Isn’t Just a Theoretical Risk
Real people have ended up in the ER because of goldenseal. One Reddit user reported near-fainting after combining it with lisinopril. Their blood pressure crashed to 85/50. Another case involved a 68-year-old diabetic whose metformin levels dropped by 25% after taking goldenseal-causing their HbA1c to jump from 6.8% to 8.2% in just four weeks. That’s not a fluke. It’s a documented interaction.
Even more alarming: the amount of berberine in goldenseal supplements varies wildly-from 0.5% to 8%. That’s a 16-fold difference. One capsule might be safe. The next one, bought from a different brand, could be dangerous. There’s no standardization. No way to know what you’re actually getting.
Merck Manual and Pharmacy Times both report goldenseal can raise INR levels in people taking warfarin, increasing bleeding risk. It can also spike cyclosporine levels in transplant patients, risking organ rejection or kidney toxicity. These aren’t rare edge cases. They’re predictable outcomes of enzyme inhibition.
How Goldenseal Compares to Other Herbs
People often think all herbal supplements are harmless. But goldenseal stands out. Compared to milk thistle-which mostly affects CYP2C9-goldenseal is far more dangerous because it hits multiple enzymes at once. Even St. John’s wort, known for causing serious interactions, works differently. It induces enzymes, making drugs less effective. Goldenseal does the opposite: it blocks them, making drugs stronger and more toxic.
A 2020 review ranked goldenseal as the third-highest risk herb for drug interactions, behind only St. John’s wort and grapefruit juice. And unlike grapefruit juice, which you can avoid by skipping the fruit, goldenseal is sold as a daily supplement. People take it for weeks. That’s long enough for enzyme inhibition to build up and cause harm.

Medications You Should Never Mix With Goldenseal
If you take any of these, skip goldenseal entirely:
- Statins: simvastatin, atorvastatin (risk of muscle breakdown)
- Blood pressure drugs: metoprolol, lisinopril, amlodipine (risk of low BP, fainting)
- Antidepressants: fluoxetine, sertraline, amitriptyline (risk of serotonin syndrome)
- Benzodiazepines: midazolam, triazolam (risk of excessive sedation)
- Diabetes meds: metformin, glipizide (risk of low or high blood sugar)
- Warfarin: risk of dangerous bleeding
- Immunosuppressants: cyclosporine, tacrolimus (risk of organ damage)
- Acetaminophen: goldenseal inhibits CYP2E1, which can reduce its safety margin and increase liver damage risk
That’s not a short list. It’s nearly half the most commonly prescribed medications in the U.S. If you take anything regularly, assume goldenseal could interfere.
What Experts Say About Goldenseal
Dr. Edzard Ernst, a leading expert in complementary medicine, called goldenseal “one of the most dangerous herbal supplements” because its interaction profile is worse than many prescription drugs. The American Academy of Family Physicians explicitly advises doctors to tell patients: don’t use goldenseal if you’re on any medication.
Even those who support herbal medicine are cautious. Dr. Tieraona Low Dog acknowledges goldenseal may help with mucosal infections-but says the lack of standardization and high interaction risk make it too risky for anyone on prescription drugs.
The FDA doesn’t approve goldenseal for any medical use. It’s sold as a supplement, meaning it’s not tested for safety or consistency. In 2021, the FDA sent warning letters to 12 companies for falsely claiming goldenseal could treat infections. That’s not marketing-it’s deception.
What to Do If You’ve Already Taken Goldenseal
If you’ve taken goldenseal and are on medications, stop immediately. Don’t wait for symptoms. The effects can last 7 to 14 days after you quit taking it. That’s how long it takes your liver enzymes to recover.
Check your meds. Use the American Society of Health-System Pharmacists’ free online CYP interaction checker. It lists 147 medications with known or possible interactions with goldenseal. If your drug is on that list, don’t take goldenseal.
Talk to your pharmacist. They’re trained to spot these interactions. Bring your supplement bottle. Many people don’t realize supplements count as medications when it comes to interactions.
Is There a Safe Way to Use Goldenseal?
Only one scenario might be low-risk: short-term use (3-5 days) for a cold or sinus infection, with no other medications taken during that time. Even then, there’s no guarantee. The NIH is currently running a $2.3 million clinical trial to study goldenseal’s interactions more precisely-results won’t be out until late 2025.
Right now, the safest answer is no. If you’re on any regular medication, goldenseal isn’t worth the risk. The benefits are unproven. The dangers are real, documented, and preventable.
What’s Changing in the Future
More doctors are learning about these risks. The American Gastroenterological Association predicts goldenseal use among patients on chronic meds will drop by 25% by 2027 as awareness grows. The FDA updated its Dietary Supplement Ingredient Database in 2023 to include specific warnings about CYP2E1 inhibition.
But the supplement industry keeps selling it. U.S. sales hit $18.7 million in 2022. And while only 3% of adults use it regularly, the majority don’t know they’re putting themselves at risk. The lack of regulation means labels lie. Products vary. And people keep taking it-thinking it’s harmless because it’s natural.
It’s not.




Comments
Himanshu Singh
December 30, 2025
Man this post saved my life honestly. I was taking goldenseal for a cold and was on metformin - didn’t realize the risk until I started feeling dizzy. Got my blood sugar checked and it was spiking. Stopped it immediately and my HbA1c went back down in 3 weeks. Everyone needs to read this.
Teresa Rodriguez leon
December 31, 2025
So let me get this straight - you’re telling me my ‘natural immune booster’ is basically a silent killer? I feel betrayed.
Sharleen Luciano
January 1, 2026
It’s not even about goldenseal - it’s about the entire supplement industry’s complete disregard for pharmacology. People treat herbal remedies like candy, but they’re pharmacologically active compounds with half-life, metabolism pathways, and enzyme kinetics. If you can’t read a CYP450 chart, you shouldn’t be self-prescribing anything beyond chamomile tea. This isn’t ‘wellness’ - it’s reckless self-medication dressed up as spirituality.
The FDA doesn’t regulate supplements because Congress is bribed by the $50 billion industry. That’s not a loophole - it’s a failure of governance. And now we have 68-year-olds crashing their glucose levels because they read a blog called ‘Herbs for the Soul’.
Dr. Ernst called it dangerous? He’s being polite. It’s a biochemical landmine wrapped in a brown paper bag labeled ‘organic’.
And don’t even get me started on the ‘it’s natural’ argument. Arsenic is natural. Botulinum toxin is natural. Nature doesn’t care if you live or die - evolution doesn’t give a damn about your sinus infection.
If you’re on any medication, your pharmacist is your real doctor. Not your yoga instructor. Not your Instagram herbalist. Not your aunt who ‘took it for years and never had a problem.’ That’s anecdotal noise, not science.
Stop romanticizing ignorance. Your liver doesn’t care if it’s ‘plant-based.’ It just wants to metabolize your meds without being sabotaged by unstandardized berberine.
Jim Rice
January 1, 2026
Actually, I’ve been taking goldenseal with my statin for 2 years and I’m fine. Maybe your liver is just weak.
Henriette Barrows
January 2, 2026
I get where you're coming from, but I think it's important to remember that people aren't trying to be reckless - they just don't know any better. I used to take it too, thinking it was safe because it’s ‘natural.’ This post opened my eyes. Thank you for sharing the real data. I’m going to talk to my pharmacist this week.
Manan Pandya
January 3, 2026
Thank you for this comprehensive breakdown. I work as a pharmacy technician in Delhi and see this exact scenario weekly - patients combining goldenseal with antihypertensives or diabetes meds, convinced it’s ‘just a herb.’ The lack of labeling and patient education is terrifying. We’ve had two cases this month alone where INR spiked after goldenseal use. This should be mandatory reading for every primary care clinic.
Aliza Efraimov
January 5, 2026
I’ve been a nurse for 18 years and I can’t tell you how many times I’ve seen patients come in with unexplained hypotension or rhabdomyolysis - and when we dig into their supplement cabinet, there’s goldenseal. Always. It’s like a silent assassin. And no one ever thinks to mention it unless you ask. ‘Oh, I just take that for my cold’ - like it’s Advil. We need warning labels on every bottle. Like cigarette packs. This isn’t hype - it’s triage-level awareness.
Nisha Marwaha
January 5, 2026
From a pharmacokinetic standpoint, the CYP3A4 and CYP2D6 inhibition profile of berberine is particularly concerning due to its non-competitive, time-dependent mechanism. The bioavailability variability across formulations - ranging from 0.5% to 8% - introduces a coefficient of variation exceeding 150%, which is clinically unacceptable for any substance co-administered with narrow-therapeutic-index drugs. The absence of batch-specific HPLC validation renders consumer-grade goldenseal pharmacologically unpredictable.
Paige Shipe
January 6, 2026
Interesting. But I think the real issue is that people don’t take responsibility for their own health. If you’re going to take something that interacts with prescription meds, you should do the research. Blaming the supplement industry is just avoidance. I’ve read the Merck Manual. I know the risks. You should too.
Kevin Lopez
January 6, 2026
CYP3A4 inhibition = bad. Goldenseal = high risk. End of story.
Amy Cannon
January 8, 2026
As someone who grew up in rural Appalachia, where ‘herbal remedies’ were passed down like family heirlooms, I find this post both alarming and deeply necessary. My grandmother swore by goldenseal for sore throats - she took it every winter, even while on her blood pressure pills. She passed away last year from kidney complications. We never connected the dots. This isn’t just about science - it’s about cultural traditions being quietly lethal. I’m going to print this out and give it to every elder in my community. Thank you for speaking truth.
Jasmine Yule
January 9, 2026
I’m so glad someone finally said this. I used to take it with my antidepressants - felt ‘more focused’ at first. Turns out I was just serotonin-overloaded. Ended up in the ER with tremors and a heart rate of 130. Scared the hell out of me. I’m now a total supplement skeptic. If it’s not FDA-approved, I don’t touch it. Period.
Greg Quinn
January 9, 2026
It’s funny how we fear pharmaceuticals but worship herbs. Both are chemicals. Both interact. Both have consequences. The difference? One has peer-reviewed data. The other has Instagram testimonials. We’re not ‘returning to nature’ - we’re just choosing ignorance over evidence. And that’s not wellness. That’s mythology with a price tag.
Lisa Dore
January 10, 2026
Just shared this with my book club. We’re all over 50 and on at least 3 meds each. Half of us were taking goldenseal. Now we’re all going to the pharmacy together next week. Group therapy for supplement ignorance - who knew?
Alex Ronald
January 11, 2026
For anyone wondering if it’s safe for short-term use - don’t. Even 3 days can inhibit CYP enzymes long enough to cause a dangerous buildup. I’ve seen it in clinical trials. The liver doesn’t reset like a phone. It takes 7–14 days, and during that time, your meds are still interacting. Better to skip it entirely. Your liver will thank you.
Write a comment