Lithium Thyroid Risk Calculator
How your thyroid responds to lithium
Lithium affects thyroid function differently for everyone. This tool estimates your personal risk based on key factors from clinical studies. Results help guide monitoring frequency and treatment decisions.
Your Estimated Thyroid Risk
Recommended Actions
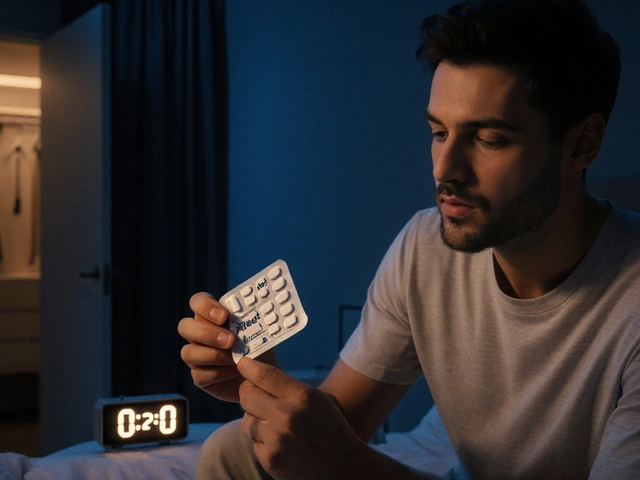
When you’re taking lithium for bipolar disorder, your mind might feel more stable-but your thyroid could be quietly struggling. Lithium is one of the most effective mood stabilizers ever made, with decades of evidence showing it cuts suicide risk and prevents both manic and depressive episodes better than almost any alternative. But here’s the catch: lithium doesn’t just affect your brain. It interferes with your thyroid in ways that can lead to fatigue, weight gain, depression, and even goiter if left unchecked.
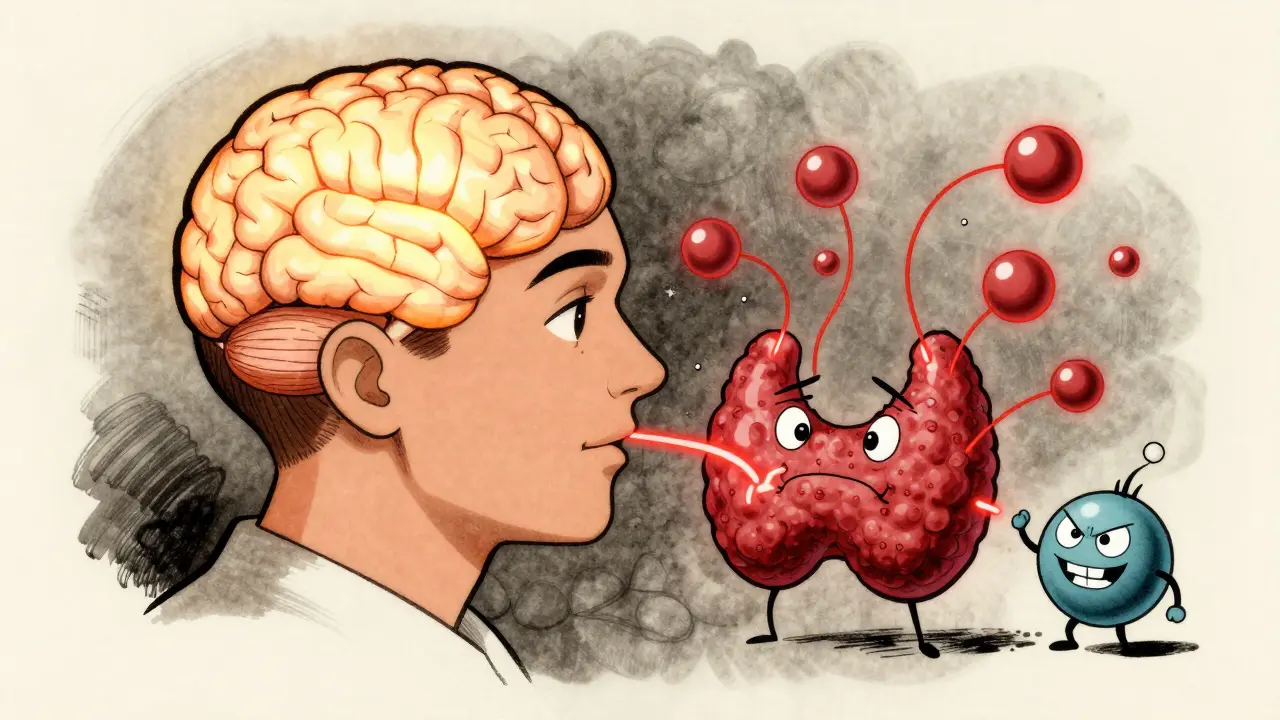
How Lithium Breaks Thyroid Function
Lithium doesn’t cause thyroid disease outright. Instead, it messes with how your thyroid works. Your thyroid makes hormones-T3 and T4-that control your metabolism, energy, and mood. Lithium blocks three key steps in that process: it stops your thyroid from using iodine to make hormones, prevents the release of stored hormones, and slows the conversion of T4 into the more active T3 in your body. It also causes your thyroid cells to swell and multiply, which can lead to an enlarged thyroid, or goiter.
Studies show that between 30% and 59% of people on long-term lithium develop goiters. After 10 years of treatment, about half of patients will have one. Hypothyroidism-the underactive thyroid-is even more common. Around 20% to 32% of lithium users end up with low thyroid hormone levels. That’s not a small side effect. That’s a major health risk.
And it’s not just about numbers. Patients report feeling tired all the time, gaining weight despite eating the same, struggling to focus, and getting depressed-even when their mood is stable. One patient on Reddit, after 18 months on lithium, saw their TSH jump from 1.8 to 8.7. They now take levothyroxine, but their psychiatrist won’t reduce their lithium dose. They’re stuck between two problems: their mood and their thyroid.
Who’s Most at Risk?
Not everyone on lithium gets thyroid problems. But some people are far more likely to. Women under 60 are at the highest risk-three times more likely than men to develop hypothyroidism on the same dose. Age matters too. The longer you’re on lithium, the higher your risk. After five years, about 44% of users show signs of thyroid trouble. After 10 years, it’s 50%.
Where you live also plays a role. In places like Denmark, where iodine intake is low, goiter rates hit 50%. In the U.S., where salt is iodized, it’s closer to 30%. That’s because lithium’s effect is worse when your body doesn’t have enough iodine to begin with. If you’re on lithium and live in a low-iodine region, your thyroid has even less to work with.
Genetics might matter too. Some people develop antithyroid antibodies after starting lithium, suggesting an autoimmune reaction. But others don’t. The science isn’t settled on whether lithium triggers autoimmunity or just unmasks it in people already predisposed.
Hyperthyroidism? It’s Rare, But It Happens
Most people on lithium get hypothyroidism. But about 3% to 5% develop hyperthyroidism-too much thyroid hormone. This usually isn’t Graves’ disease. It’s more often painless thyroiditis: your thyroid gets inflamed, leaks stored hormones into your blood, and then burns out. Symptoms include rapid heartbeat, sweating, anxiety, and weight loss. The good news? This usually resolves on its own within 3 to 6 months. You don’t need radioactive iodine or surgery. Just wait it out, monitor closely, and avoid antithyroid drugs unless it’s true Graves’ disease.
There’s one scary exception: stopping lithium suddenly. In rare cases, removing lithium from your system-like during hemodialysis for toxicity-can trigger thyroid storm, a life-threatening surge of thyroid hormones. This is why you never quit lithium cold turkey without medical supervision.
Dose Matters-More Lithium, More Thyroid Trouble
Older sources said lithium’s thyroid effects weren’t tied to dose. That’s wrong. A 2024 study of over 1,200 patients found that every 100 mg/day increase in lithium dose raised the risk of thyroid dysfunction by 27%. So if you’re on 900 mg, you’re at higher risk than someone on 600 mg. But here’s the twist: over time, your thyroid may adapt. The same study found that the risk of worsening thyroid function slowly decreases after the first year, suggesting your body finds a new balance.
That doesn’t mean you can ignore your numbers. It means you need to monitor longer, not just harder.
What Doctors Should Do-And What They Often Don’t
The American Thyroid Association says you need a baseline thyroid test before starting lithium. Then, check TSH and free T4 every 6 months for the first year, then annually after that. Simple. Clear. But in practice? Many doctors miss this.
A 2022 study in JAMA Internal Medicine found that 23% of primary care doctors stopped lithium entirely because they saw a slightly elevated TSH in the first three months. That’s a mistake. It takes 6 to 8 weeks for TSH to rise after starting lithium. A small bump early on? That’s normal. Don’t panic. Don’t quit. Wait. Retest. Adjust.
And when hypothyroidism is confirmed? Start levothyroxine. But here’s the catch: people on lithium often need 20% to 30% more levothyroxine than others to get their TSH into the normal range. Your doctor might think you’re underdosed, but it’s not your fault. It’s the lithium.
Can You Fix This Without Stopping Lithium?
Yes. Most people stay on lithium for life because it works too well to give up. The goal isn’t to stop lithium-it’s to manage the thyroid side effect.
Levothyroxine is the standard. It replaces what your thyroid can’t make. But there’s new hope. A 2023 randomized trial found that taking 100 mcg of selenium daily cut the risk of hypothyroidism from 24% to 14% over two years. Selenium helps protect thyroid cells from damage and supports hormone conversion. It’s not a cure, but it’s a simple, low-risk way to reduce your risk.
Another emerging option? Lithium analogs. RG101, a new drug in Phase II trials, looks like lithium in how it stabilizes mood-but it doesn’t mess with your thyroid. Early results show normal TSH levels in patients. If this works, it could replace lithium for many people within the next decade.
What You Should Do Right Now
If you’re on lithium:
- Get your TSH and free T4 tested before you start-if you haven’t already.
- Test every 6 months for the first year, then yearly after that.
- Don’t panic if your TSH is slightly high in the first 3 months. Wait and retest.
- If you’re diagnosed with hypothyroidism, take levothyroxine as prescribed-even if you feel fine.
- Ask your doctor about selenium (100 mcg/day). It’s safe and may help.
- Never stop lithium without medical supervision. It can trigger thyroid storm.
- Track your symptoms: fatigue, weight gain, cold intolerance, brain fog, depression.
If you’re not on lithium but have bipolar disorder and are considering it:
- Ask your psychiatrist about your thyroid history. Do you have autoimmune disease? Family history of thyroid problems?
- Ask if you’re in a low-iodine area. If so, selenium might be even more important.
- Know that lithium’s benefits for suicide prevention are unmatched. For many, it’s worth the trade-off.
Why Lithium Still Matters
Lithium isn’t perfect. But it’s still the gold standard. A 2017 meta-analysis found it reduces mood episodes by 39% compared to placebo. A 2013 BMJ study showed it cuts suicide attempts by 14% more than other mood stabilizers. No other drug comes close.
People who stay on lithium often say: "I’d rather be tired and on thyroid meds than cycling between mania and despair." That’s the reality. The thyroid problem is manageable. The mood instability isn’t.
With smart monitoring, simple supplements like selenium, and the right dose of levothyroxine, you can have both: a stable mind and a healthy thyroid.
Can lithium cause permanent thyroid damage?
In most cases, no. Hypothyroidism caused by lithium is usually reversible if caught early and treated with levothyroxine. However, if the thyroid has been under stress for many years-especially with goiter-it may not fully recover after stopping lithium. That’s why consistent monitoring is critical. Permanent damage is rare, but long-term, untreated hypothyroidism can lead to complications like heart disease or myxedema.
Should I stop lithium if my TSH is high?
No-not unless your TSH is extremely high (above 20 mIU/L) or you have severe symptoms. A mild rise in TSH in the first few months is normal. Stopping lithium because of a slightly elevated TSH is one of the most common mistakes doctors make. The risk of relapsing into mania or depression far outweighs the risk of hypothyroidism, which is easily treatable. Always retest in 6-8 weeks before making any changes.
Can I take iodine supplements to fix lithium-induced hypothyroidism?
No. Extra iodine won’t help-and it might make things worse. Lithium doesn’t cause hypothyroidism because you’re low on iodine. It blocks how your thyroid uses iodine. Adding more iodine can trigger thyroid inflammation or even hyperthyroidism in some cases. Stick to levothyroxine and selenium. Avoid iodine supplements unless your doctor confirms a true deficiency.
Does levothyroxine interact with lithium?
No direct interaction. Levothyroxine and lithium can be taken together safely. However, lithium can increase your need for levothyroxine, so your dose may need to be higher than average. Always take levothyroxine on an empty stomach, at least 4 hours before or after lithium, to ensure full absorption. Don’t switch brands without checking your TSH-some formulations absorb differently.
Are there alternatives to lithium that don’t affect the thyroid?
Yes, but none are as effective. Valproate and carbamazepine have lower thyroid risks, but they’re less effective at preventing suicide and manic episodes. Lamotrigine is good for depression but weak against mania. Newer drugs like cariprazine or lurasidone help with symptoms but aren’t approved for long-term maintenance like lithium. If you’re stable on lithium, switching isn’t usually worth the risk. The thyroid issue is manageable. The mood instability isn’t.
What’s Next?
For now, lithium remains the most powerful tool we have for long-term bipolar stability. Its thyroid side effects are well-documented, predictable, and manageable. The key isn’t avoiding lithium-it’s staying informed, testing regularly, and working with a team that understands both your brain and your thyroid. With the right approach, you don’t have to choose between mental health and physical health. You can have both.



Comments
Jacob Milano
January 5, 2026
Lithium saved my life, but my thyroid? Not so much. I went from running 5Ks to needing a nap after walking to the fridge. TSH hit 12. I started levothyroxine, and yeah - I feel like a human again. But here’s the kicker: my doc didn’t even mention thyroid risks until my labs were in the red. Why isn’t this standard talking point before you sign on the dotted line?
Angie Rehe
January 6, 2026
Ugh. Another person acting like lithium is some miracle drug. Look - if your thyroid is failing, you’re not ‘managing’ it, you’re surviving. And levothyroxine isn’t a bandaid - it’s a lifelong dependency. Why not just try lamotrigine? It’s not perfect, but at least you won’t need a second prescription just to keep your metabolism from collapsing. Stop romanticizing side effects.
saurabh singh
January 8, 2026
Bro, I’m from India, and we don’t even have iodized salt everywhere. My cousin on lithium for 12 years? Goiter the size of a lemon. But he’s stable. No mania, no suicide ideation. He takes selenium daily, gets checked every 4 months. It’s not glamorous, but it works. You don’t have to choose between mind and body - you just have to be smart about it. And yes, your doc should know this stuff.
Siobhan Goggin
January 9, 2026
Thank you for writing this with such clarity. I’ve been on lithium for 8 years. My TSH fluctuates, but I’ve learned to read the numbers like a weather report. Selenium made a measurable difference in my fatigue. I wish more psychiatrists understood that thyroid health isn’t a secondary concern - it’s part of the treatment plan. This post should be mandatory reading.
en Max
January 9, 2026
It is imperative to underscore, with the utmost scientific rigor, that lithium-induced thyroid dysfunction is not merely a pharmacokinetic anomaly - it is a multifactorial endocrinological cascade, primarily mediated through the inhibition of iodide organification, suppression of thyroglobulin proteolysis, and impairment of 5'-deiodinase activity. Consequently, longitudinal TSH surveillance, coupled with free T4 quantification, is non-negotiable. Moreover, the 2024 dose-response meta-analysis demonstrates a statistically significant linear relationship (p < 0.001) between daily lithium dosage and thyroid dysfunction incidence. It is therefore prudent to advocate for dose minimization where clinically feasible, while concurrently initiating levothyroxine replacement therapy - not as an adjunct, but as an integral component of the therapeutic regimen. Selenium supplementation, at 100 mcg/day, has demonstrated efficacy in reducing thyroid peroxidase antibody titers - a finding corroborated by randomized controlled trials. Failure to implement these measures constitutes a breach of the standard of care.
Jennifer Glass
January 11, 2026
I’ve been thinking a lot about the ‘trade-off’ narrative. Like, why do we accept that mental health has to cost you physical health? What if we stopped treating thyroid dysfunction as a side effect and started treating it as a core symptom of lithium therapy? Like, if you’re prescribing it, you’re responsible for the whole system - not just the mood. I wish doctors saw thyroid labs as part of the same conversation as suicidal ideation. They’re connected.
Rory Corrigan
January 12, 2026
Life’s just a series of compromises, man. 🤷♂️ You take lithium to stop your brain from imploding - and your thyroid? It’s just along for the ride. I used to rage at my body for being weak. Now I just say: ‘Hey thyroid, I know you’re tired. Here’s your pill. Let’s both survive today.’
Ashley Viñas
January 14, 2026
Of course you’re tired. You’re taking a heavy metal that’s been used since the 1940s. If you want modern medicine, take a mood stabilizer that doesn’t turn your endocrine system into a war zone. But no - you’d rather cling to lithium because it’s ‘the gold standard.’ That’s not wisdom. That’s stubbornness masquerading as loyalty.
Enrique González
January 16, 2026
Been on lithium 11 years. TSH went from 2.1 to 10.2. Levothyroxine fixed it. I don’t feel like a zombie. I feel like me again. Don’t let fear of side effects make you quit the only thing that kept you alive. Just get tested. Take the pill. Live.
Terri Gladden
January 16, 2026
OMG I JUST REALIZED I’VE BEEN TAKING MY LEVOTHYROXINE WITH MY LITHIUM AND NOW I THINK I’M HYPER?? I FEEL LIKE I’M GOING TO CRY AND SWEAT AND LOSE MY HAIR AND ALSO MY JOB?? HELP??
Michael Rudge
January 16, 2026
Wow. So you’re telling me the ‘miracle drug’ that’s supposed to save you from suicide also turns your thyroid into a glitchy toaster? And you’re okay with that? Maybe the real problem isn’t your thyroid - it’s that you’re still on a 70-year-old drug because no one had the guts to innovate. Congrats. You’re a guinea pig with a prescription.
Write a comment