Every day, pharmacists dispense billions of generic medications. In 2023, 75% of all prescriptions filled in the U.S. were generics. That’s over 5.8 billion prescriptions. And yet, pharmacists contribute less than 3% of the adverse event reports submitted to the FDA. Why? Because reporting isn’t just about knowing the rules-it’s about breaking through systemic barriers that make it hard to speak up, even when something’s wrong.
What Exactly Are Pharmacists Supposed to Report?
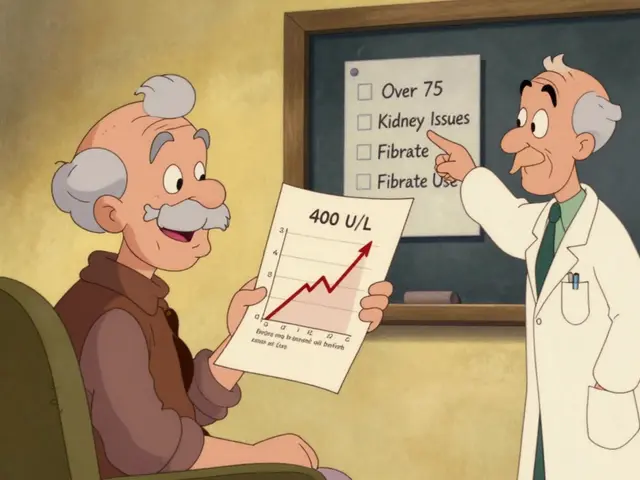
Pharmacists aren’t just filling prescriptions. They’re the last line of defense before a patient swallows a pill. That means they see problems others don’t. A patient comes in complaining their new generic blood pressure pill isn’t working like the old one. Another says they’re dizzy after switching to a different manufacturer’s version of the same drug. These aren’t random complaints-they’re signals. The FDA calls these potential issues therapeutic inequivalence. That’s when a generic drug performs differently in real life than it should, even though it passed lab tests. It might absorb too slowly. Too fast. Or not at all. The patient doesn’t know the difference. But the pharmacist does. And the FDA says: if you see it, report it. Serious adverse events include anything that’s life-threatening, causes hospitalization, leads to permanent disability, or requires urgent medical intervention. But you don’t need to be 100% sure the drug caused it. The FDA’s 2023 guidance is clear: report even if you’re uncertain. A vague report like “patient had a bad reaction” won’t cut it. You need details: the patient’s age, the exact drug name, the NDC code, the lot number, and what happened. Without those, your report gets ignored.Why Is This So Hard to Do?
Time is the biggest blocker. In a 2023 survey of community pharmacists, 68.4% said they didn’t report because they were too busy. Filling prescriptions, answering questions, managing insurance issues-it’s nonstop. Filling out a MedWatch form takes 15 to 20 minutes. Most don’t have that time. Then there’s confusion. Pharmacists aren’t trained to be detectives. When a patient says, “This generic made me sick,” how do you know if it’s the drug, the patient’s condition, or something else? 76.3% of pharmacists in a 2023 ASHP survey said they struggle to tell the difference between a drug problem and a patient problem. And here’s the worst part: you often don’t even know which manufacturer made the pill. Generic drugs look identical. The label doesn’t say who made it. The pharmacy system might not either. So when you try to report, you’re stuck guessing. That’s why 41.7% of pharmacists say they avoid reporting because they can’t identify the maker. There’s also fear. What if you report and nothing happens? What if you’re wrong? The system feels broken. In 2022, only 2.3% of all FDA reports came from pharmacists-even though we’re the ones who handle the drugs. Doctors, who prescribe fewer generics, file nearly 30% of reports. Manufacturers? They file nearly 70%. Why? Because they’re legally required to report. Pharmacists? Not so much.Legal Reality: You’re Not Required-But You’re Responsible
There’s no federal law forcing pharmacists to report. The FDA asks. They encourage. They beg. But they can’t make you. The 1984 Hatch-Waxman Act and the 2011 Supreme Court case PLIVA v. Mensing made it so generic manufacturers can’t change warning labels-even if they know there’s a problem. That means the burden of spotting issues falls on the people who see patients every day: pharmacists. But professional responsibility isn’t the same as legal obligation. The American Society of Health-System Pharmacists (ASHP) says adverse event reporting is a fundamental professional responsibility. The California Board of Pharmacy says pharmacists must have a system to identify and report drug problems. Four states-California, Illinois, Massachusetts, and New York-have made reporting mandatory for serious events. The rest? It’s up to you. That’s the tension. Legally, you’re free. Ethically? You’re on the hook.
What Happens When You Report?
You fill out Form 3500 on the FDA’s MedWatch portal. You pick “generic drug concern” and choose whether it’s about therapeutic inequivalence, manufacturing quality, or labeling. You enter the NDC, lot number, patient info (if available), and a clear description of what happened. Then what? The FDA’s Office of Generic Drugs reviews it. They look for patterns. One report? Might be noise. Five reports about the same generic from different states? That’s a red flag. In 2022, pharmacist reports led to 147 generic drugs being re-evaluated. Twelve of those led to official warnings to doctors and patients. One study found that 63% of safety signals in the FDA’s database were first spotted by pharmacists who noticed the same issue across multiple patients. That’s not luck. That’s expertise. And here’s the kicker: reports from pharmacists are more likely to lead to action than reports from patients. Why? Because pharmacists understand dosing, interactions, and bioequivalence. A patient says, “I feel weird.” A pharmacist says, “The patient’s INR spiked after switching from Brand X to Generic Y. Both are labeled as warfarin 5mg. But the absorption profile appears inconsistent.” That’s actionable.How to Report Without Getting Overwhelmed
You don’t need to report every odd symptom. But you should report anything that’s:- Unexpected (not listed in the drug’s side effects)
- Recurring (same issue with multiple patients on the same generic)
- Severe (hospitalization, serious injury, death)
- Linked to a switch (patient did fine on brand, got worse on generic)
Why This Matters More Than You Think
Generic drugs save the U.S. healthcare system $370 billion a year. That’s huge. But if those drugs aren’t working as they should, patients suffer. And the system loses trust. When pharmacists don’t report, the FDA can’t see the real-world problems. They rely on manufacturers to self-report. But manufacturers have a conflict: they don’t want to admit their product is flawed. They don’t want recalls. They don’t want lawsuits. So they downplay issues. Pharmacists are the only ones who have no stake in the outcome. We don’t make the drug. We don’t profit from it. We just hand it to the patient. That’s why our reports carry weight. The FDA’s own data shows that reports from pharmacists are more likely to trigger investigations. They’re more detailed. More specific. More credible. If you don’t report, you’re letting the system rely on guesses. And someone’s health is on the line.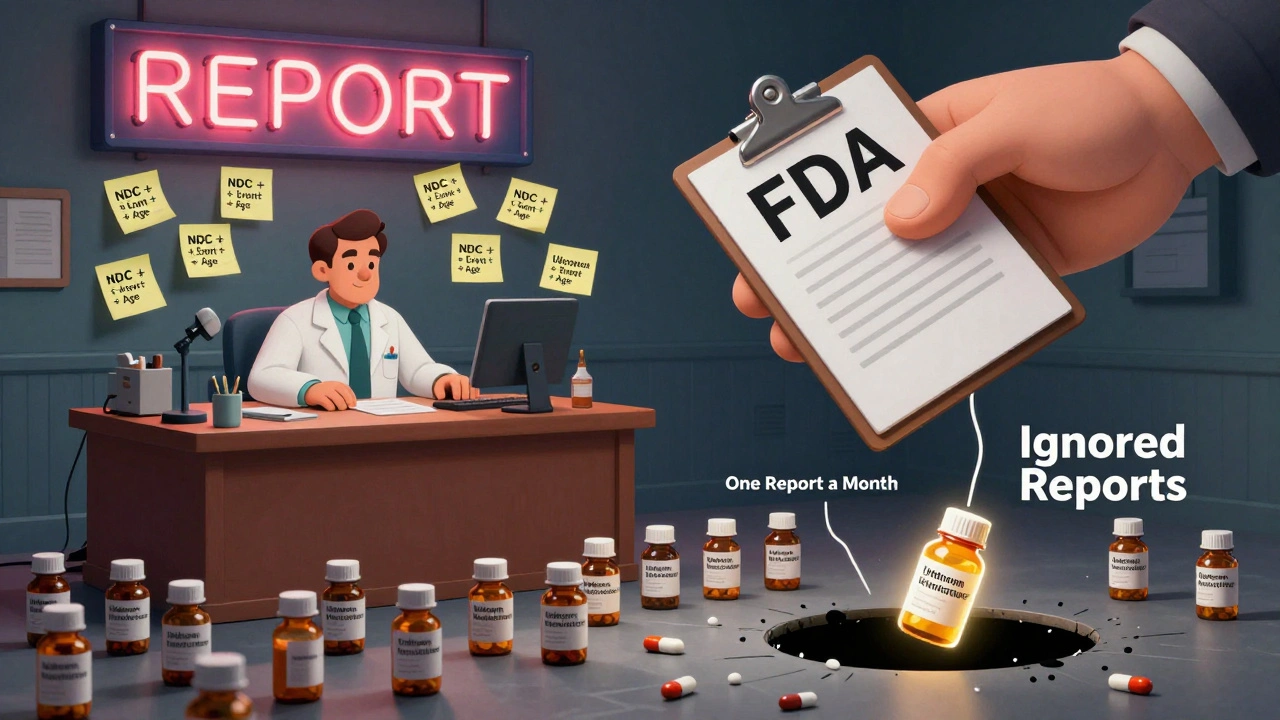
What You Can Do Today
1. Know your NDC codes. Keep a quick reference list of common generics and their manufacturers. 2. Ask patients. After switching to a generic, ask: “How’s it working for you compared to before?” Don’t assume it’s fine. 3. Document everything. Even if you don’t report, write it down. Date, drug, patient reaction. That’s your professional record. 4. Report the pattern, not the single event. One odd reaction? Maybe coincidence. Three in a month? That’s a signal. 5. Use the FDA’s updated MedWatch portal. It now has a dedicated “generic drug concern” category. Use it. You don’t need to be a hero. You just need to be consistent. One report a month. That’s it. If every pharmacist did that, the FDA would have 300,000 new reports a year. That’s enough to catch problems before they hurt thousands.Frequently Asked Questions
Are pharmacists legally required to report generic drug problems to the FDA?
No, federal law does not require pharmacists to report adverse events or generic drug problems. The FDA encourages reporting through the MedWatch program, but it’s voluntary. However, some states-including California, Illinois, Massachusetts, and New York-have made reporting mandatory for serious adverse events. Professional organizations like ASHP consider reporting a core ethical responsibility, even if it’s not legally required.
What kind of generic drug problems should I report?
Report any issue that seems unusual or potentially dangerous. This includes therapeutic inequivalence-when a generic drug doesn’t work the same way as the brand or a previous version-especially if patients report unexpected side effects, lack of effectiveness, or worsening symptoms after switching. Also report serious adverse events like hospitalizations, life-threatening reactions, or permanent disability. Even if you’re unsure the drug caused it, report it. The FDA says: better to report and be wrong than to miss a pattern.
How do I know which manufacturer made the generic drug?
Check the National Drug Code (NDC) on the prescription label or packaging. The NDC includes the manufacturer identifier. If the label doesn’t show it, your pharmacy’s system should. If you’re still unsure, call the wholesaler or check the FDA’s NDC directory online. Even if you can’t confirm the manufacturer, report what you know-specify that the manufacturer is unknown. The FDA can still analyze the pattern.
Is it worth reporting if I only see one patient with a problem?
Yes, but only if the event is serious or unexpected. One isolated case might be a coincidence. But if the reaction is severe-like chest pain, severe dizziness, or a drop in blood pressure-and it’s not listed as a common side effect, report it. The FDA looks for clusters. If three other pharmacists report the same issue with the same generic, they’ll investigate. Your report could be the first clue.
What if I report and nothing happens?
That’s normal. Most reports don’t lead to immediate action. But the FDA’s system works by accumulating data. Thousands of small reports create patterns. One report might not change anything. But if 100 pharmacists report the same issue, the FDA launches a formal review. Your report contributes to a larger safety net. It’s not about immediate results-it’s about collective vigilance.
Next Steps for Pharmacists
If you’re unsure where to start, begin with these three actions:- Complete the FDA’s free MedWatch training module for healthcare professionals-it’s under 30 minutes and available online.
- Ask your pharmacy manager if you can add a simple checklist to your workflow: “Did the patient switch generics? Did they report a change in how they feel?”
- Start tracking one generic drug per week. If you notice the same problem twice, report it. That’s all it takes to become part of the solution.




Comments
Joanne Rencher
December 3, 2025
Wow, so now pharmacists are supposed to be detectives, data entry clerks, and moral guardians all at once? Cool. Meanwhile, I’m waiting for my blood pressure med to not make me feel like a zombie, and no one’s asking if the damn thing even works. Just tell me where to click and stop making me feel guilty for being busy.
Adrianna Alfano
December 3, 2025
ok so i just had a patient come in crying because her generic lexapro made her feel like she was underwater and she couldnt breathe? she switched from brand and now shes scared to take anything. i tried to report it but the system didnt even show the manufacturer and i had to call 3 diff wholesalers just to get the ndc. why is this so hard?? and why do we get zero support for this? the fda just says 'report it' like its easy. its not. its a nightmare. and no one cares until someone dies.
Casey Lyn Keller
December 5, 2025
Let me guess-the real reason pharmacists don’t report is because the FDA is just a paper tiger. They take your reports, file them in a digital drawer labeled 'Maybe Later,' and then turn around and approve ten more generics with the same NDC code from the same factory in India. We’re not lazy. We’re just tired of shouting into a void.
Stacy Natanielle
December 6, 2025
While I appreciate the moral imperative outlined here, the structural inadequacies of the current reporting framework cannot be overstated. The burden of documentation, the absence of standardized manufacturer identification protocols, and the lack of institutional support render this 'professional responsibility' functionally untenable. Furthermore, the reliance on voluntary compliance in a high-volume, low-reward environment constitutes a systemic failure of public health governance.
kelly mckeown
December 7, 2025
i’ve been doing this for 12 years and i’ve only ever reported twice. not because i don’t care, but because i don’t have 20 minutes between 12 patients and 3 insurance calls. if the system made it one click, i’d do it every week. just give us a button. that’s all. a simple button. and maybe a thank you.
Tom Costello
December 8, 2025
One of the most underappreciated roles in healthcare. Pharmacists are the only ones who actually see the patient after the prescription leaves the doctor’s office. If we’re going to ask them to be the eyes and ears of the FDA, we need to give them tools-not guilt. A simple mobile app with pre-filled fields, auto-populated NDCs from the pharmacy system, and one-click submission. Done. No more excuses.
dylan dowsett
December 9, 2025
You’re all missing the point. This isn’t about reporting-it’s about control. The FDA doesn’t want you reporting. They want manufacturers to control the narrative. They know if pharmacists started reporting consistently, they’d have to shut down half the generics on the market. So they make it impossible. That’s not negligence. That’s policy.
Chad Kennedy
December 11, 2025
I’ve seen this happen. Patient switches to generic. Gets dizzy. Comes back. I write it down. Nothing happens. Then the same thing happens again with another patient on the same batch. Still nothing. Then a third. Still nothing. So I stopped writing it down. Why? Because it doesn’t matter. No one cares. And I have kids to feed.
Siddharth Notani
December 13, 2025
As a pharmacist from India, I can confirm: this issue is global. In our country, generics are 95% of prescriptions. But we have no centralized reporting system. We rely on paper forms. Many pharmacists don’t even know what MedWatch is. Education and infrastructure are the real barriers-not laziness.
Cyndy Gregoria
December 13, 2025
Hey-you can do this. One report a month. That’s it. Just one. Pick a patient who switched. Ask them how they’re feeling. Write it down. Submit it. You don’t need to be perfect. You just need to start. The system isn’t broken because you’re lazy. It’s broken because no one shows up. Be the one who does.
Akash Sharma
December 13, 2025
It’s interesting to note that the discrepancy in reporting rates between pharmacists and manufacturers is not merely a matter of legal obligation but also of institutional incentives. Manufacturers are financially motivated to suppress adverse event data, while pharmacists, despite being on the front lines, lack both the technological infrastructure and the organizational backing to systematically collect and submit data. Furthermore, the FDA’s reliance on voluntary reporting creates a selection bias-only the most motivated or the most outraged pharmacists report, skewing the data toward extreme cases and missing the subtle, widespread patterns of therapeutic inequivalence that occur daily. This systemic blind spot undermines the entire pharmacovigilance framework, and until pharmacists are integrated into a structured, incentivized, and technologically supported reporting network, we are merely tinkering at the edges of a much larger problem.
Justin Hampton
December 14, 2025
Oh please. You think your one report matters? The FDA gets 10,000 reports a week. Yours is just noise. And if you think generic drugs are the problem, look at the real culprit: the FDA approves them based on lab tests that have nothing to do with real human bodies. That’s the real scandal. Not you not reporting. The system is rigged.
Pooja Surnar
December 15, 2025
Pharmacists are lazy and don’t want to do their job. If you can’t be bothered to report a life-threatening reaction, you shouldn’t be holding a license. People are dying because you’re too busy scrolling on your phone. Wake up. This isn’t a suggestion-it’s your duty. Stop making excuses.
Gerald Nauschnegg
December 17, 2025
So wait-let me get this straight. I’m supposed to report every time a patient says their generic makes them feel weird? What if they’re just stressed? What if they didn’t sleep? What if they’re on six other meds? How am I supposed to know? And if I report everything, I’ll be filing 50 forms a day. Then what? I get a medal? Or just more work?
Write a comment